INTRODUCTION
Concussions are a common problem in pediatric patients with estimates of 2 million outpatient visits and nearly 3 million emergency department visits occurring for concussion-related symptoms in 2005 to 2009.1 Injuries can be due to a multitude of etiologies, including vehicular trauma and sports. Defined as a brief disturbance of brain function due to a traumatic inciting event, concussions are thought to be due to abnormal neurometabolic and vascular response, which contributes to mood, cognitive, physical, and sleep symptoms. Recovery windows are variable with high rates of spontaneous recovery over 10 to 30 days. Although most patients will recover without incident, during this recovery period, disordered metabolism leaves the brain less able to respond to the injury, increasing the vulnerability for longer-lasting symptoms.2
Once children have been removed from scenarios where reinjury may occur, such as restriction from activities/sports, receiving timely care and education is important. Families need to know that continuing sports while still symptomatic can lead to increased or more severe concussive symptoms and longer recovery times.3 Without activity restrictions, children are at risk for a second concussive injury, which can also produce worsening symptoms and prolonged recoveries that may potentially result in death.4–6 In addition, a subset of patients will have prolonged symptoms that may benefit from targeted rehabilitation or management.1 The literature is not supportive of pharmacological or alternative medicine treatments.7 Evidence-based guidelines recommend that patients who are slow to recover be referred to a concussion specialty clinic.8,9 Providing a multidisciplinary evaluation can help identify underlying factors that may be contributing to persistent symptoms and identify targets for treatment. Such an assessment may involve a team of healthcare professionals, including a sports medicine specialist or physician with similar expertise, an athletic trainer, a physical therapist, a neuropsychologist, and, in certain cases where symptoms persist for over a month, a psychologist or psychiatrist to provide behavioral management.
As families leave urgent cares or emergency departments with a diagnosis of concussion in their child, discharge instructions may include information for them to follow-up with their primary care physician. If families are not connected to the medical system or their primary care provider is not able to address ongoing concerns, they may resort to internet searches to find local care options. A previous study in Canada using internet searches showed that the number of concussion care providers varied widely across the different provinces with a wide spectrum of clinicians providing care and services provided10; the group used similar methodology to look at services provided in the United States based on each state, recognizing that personnel and services vary.11 Beyond this, literature gaps exist in understanding access to optimal, multidisciplinary concussion care based on where a patient lives. There is also difficulty in assessing the quality of care, especially for pediatric patients. This study aimed to evaluate access to optimal concussion care based on a patients’ geography with the hypothesis that there is differential access across the United States. To do so, we employed a novel strategy using internet web searches to find local care, mimicking what families might do in different parts of the country. The primary outcomes were to evaluate 2 factors: access and optimal care. Access was defined by the distance to clinic and by the ability of the site to see pediatric patients. Optimal care was defined by ability to self-refer and by the presence of multidisciplinary care. Data were evaluated based on defined geographic regions and rural versus metropolitan areas for states.
METHODS
The search methodology used for this study is like those previously published that used free, publicly available web sites,10,11 similar to what families may search when looking for concussion care. As this information is publicly available, this is not human subjects research and does not require approval by the institutional review board.
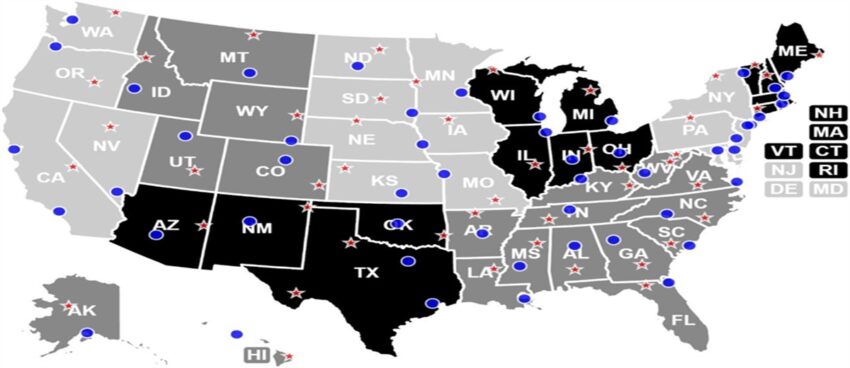
The “Metropolitan and Micropolitan Statistical Areas of the United States” map created by the US Census Bureau in 2018 was used to define metropolitan, micropolitan, and rural areas. To be delineated as a metropolitan statistical area, a county had to contain at least 1 urbanized area with a population of 50 000 or more, along with a “high degree of economic and social integration.” Micropolitan areas were designated using the same criteria, but containing an urbanized area with a population of 10 000 to 50 000. Any areas not meeting these requirements were designated as rural. For this study, 1 metropolitan and 1 rural area for each of the 50 US states was selected (Figure 1). In each state, the metropolitan area that contained that state’s most populated city was selected. The rural area was selected for each state based on maximum distance from nearby metropolitan or micropolitan areas, both within the same state and across state lines. However, exceptions did exist based on census and geography. An additional metropolitan area was selected for California, and additional metropolitan and rural areas were selected for Texas due to the large populations and sizes of these states. If a state did not contain any rural areas, 1 micropolitan area was selected for analysis in its place (Connecticut and Hawaii). However, if a state contained neither rural nor micropolitan areas (Delaware, Massachusetts, New Jersey, and Rhode Island), only a metropolitan statistical area was selected. Figure 1 displays the geographic representation of metropolitan and rural areas across the country.
Geographic visualization of the metropolitan and rural areas identified across the country with regions outlines as well.
To change the location to the desired metropolitan, micropolitan, or rural area for an internet search, the Google web page was manipulated by right clicking and selecting “inspect.” Next, under the “sensors” section, “location,” “overrides,” and subsequently “other” were then selected before the latitude and longitude of the rural or metropolitan area of interest were entered. After refreshing the web page, the option to update location was selected before continuing with the search. To perform the search itself, the phrase “concussion care near me” was used for each area. The first nonadvertisement results were selected, including Google maps results, with a maximum of 5 results being chosen. Results did not need to be in the same state as the area; for example, selected results could also be in other states or countries. From there, the page result was systematically reviewed for the following information: the institution’s name, phone number, general information about concussions, self-referral through the institution, multidisciplinary concussion care, sees pediatric patients, distance from search coordinates, medical specialties available for care, telehealth availability, and any stated guidelines for patients returning to sports. Pediatric patients were defined as less than 18 years old, but this was more often listed on the web site as pediatric without a defined age range. Results were said to contain self-referral if the resulted web site offered concussion care and provided information for accessing this care (phone number, online appointment scheduler, contact email, business hours, etc). Care was defined as multidisciplinary if it contained at least 1 medical specialty capable of prescribing medication and coordinating a treatment plan and at least 1 other allied healthcare discipline such as physical therapy, occupational therapy, or athletic training. Information was collected into a Qualtrics survey for further analysis. Factors evaluated for access included distance to clinic and ability to see pediatric patients. Factors evaluated for optimal care include ability for self-referral and availability of multidisciplinary care; these were considered optimal attributes as early referral to multidisciplinary specialty care has been associated with faster recovery12 and self-referral systems can bypass scheduling difficulties experienced in health care.
If a result linked to a web page of a clinic system with multiple locations, the location closest to the search coordinates was used. If the first 5 nonadvertisement search results include a duplicate web page listing more than 1 clinic location, the information would be entered into the survey, along with the location of the second closest clinic. However, if the duplicate web page occurred more than once within the first 5 nonadvertisement search results and did not have a second location, it would not be entered into the survey and the sixth nonadvertisement result would take its place. Finally, if a duplicate web page resulted from new search coordinates, it would be entered into the survey as a unique entry. Figure 2 provides an overview of the processing steps when encountering a web site to determine if it should be included or not.

Simplified schematic of web site processing.
Statistics
Data were sampled by metropolitan, micropolitan, or rural areas by state and then organized into regions, as defined in Figure 1. For sample web sites where there was an unknown variable, that data point was counted as no as a family would not have access to that information via a reasonable search that they might perform. For statistical analysis, Fisher exact test was performed when comparing across groups. Significance was set for a P-value ≤0.05.
RESULTS
In total, 490 sites were surveyed with all 50 states represented. Metropolitan areas represented 52.4% (n = 257) and rural areas represented 47.6% (n = 233). As seen in Table 1, the data are organized based on primary outcomes of access and optimal care where access represents (1) distance and (2) whether the clinic sees pediatric patients, whereas optimal care represents (1) self-referral and (2) multidisciplinary care.
Breakdown by Geographic Location and Primary Outcomes of Access and Optimal Care
| Geographic Breakdown | Access | Optimal Care | ||
| Distance | Clinic Sees Pediatric Patients, n (%) | Self-Referral, n (%) | Multidisciplinary, n (%) | |
| National (n = 490) | 295 (60.2) | 157 (32.0) | 457 (93.3) | 144 (29.4) |
| Regions | ||||
| Alaska (n = 10) | 5 (50.0) | 3 (30.0) | 10 (100) | 1 (10.0) |
| Far West (n = 43) | 28 (65.1) | 10 (23.2) | 41 (95.3) | 12 (27.9) |
| Hawaii (n = 10) | 9 (90.0) | 1 (10.0) | 9 (90.0) | 1 (10.0) |
| Rocky Mountain (n = 50) | 23 (46.0) | 12 (24.0) | 50 (100) | 17 (34.0) |
| Southwest (n = 50) | 26 (52.0) | 21 (42.0) | 42 (84.0) | 6 (12.0) |
| Plains (n = 70) | 40 (57.1) | 20 (28.6) | 70 (100) | 20 (28.6) |
| Great Lakes (n = 50) | 32 (64.0) | 18 (36) | 50 (100) | 10 (20.0 |
| Mideast (n = 40) | 24 (60.0) | 14 (35.0) | 31 (77.5) | 21 (52.5) |
| New England (n = 47) | 28 (59.6) | 12 (25.5) | 43 (91.5) | 14 (29.8) |
| Southeast (n = 120) | 80 (66.7) | 46 (38.3) | 111 (92.5) | 42 (35.0) |
| Area type | ||||
| Metropolitan (n = 257) | 244 (94.9) | 83 (32.3) | 235 (91.4) | 68 (26.5) |
| Rural (n = 233) | 51 (21.9) | 74 (31.8) | 222 (95.3) | 76 (32.6) |
Significant differences are noted between regions within optimal care for self-referral (P P = 0.0025). By area, significant differences exist for distance (P
Access: Distance to Care
Nationally, 230 of the 490 surveyed results (46.9%) were within 10 miles of searched locations, 65 (13.3%) within 50 miles, 46 (9.4%) within 100 miles, 51 (10.4%) within 200 miles, 86 (17.6%) within 500 miles, 6 (1.2%) within 1500 miles, and 6 (1.2%) within an unknown distance. When evaluating regions, it was seen that an average of 50.2% of results were within 10 miles of the searched location. Hawaii had the highest proportion (90%) of results within 10 miles, whereas the Mideast had the lowest (32.5%) within 10 miles. When separating search locations by metropolitan versus rural designation, significant differences exist based on distance (P
Access: Clinic Sees Pediatric Patients
Nationally, 157 (32.0%) of the 490 results saw pediatric patients. When separating by region, an average of 29.6% of results saw pediatric patients. The Southwest had the highest proportion (44%), whereas Hawaii had the lowest (10%). For comparison of areas, no significant difference was detected as 83 (32.3%) of metropolitan sites see pediatric patients versus 74 (31.8%) of rural areas. Two metropolitan locations did not include whether they saw pediatric patients.
Optimal Care: Self-referral
Nationally, 457 (93.3%) of the results offered self-referral, 27 (5.5%) did not, and the remaining 6 (1.2%) could not be allocated to either category. Significant differences were detected between regions (P
Optimal Care: Multidisciplinary Care
Nationally, 144 (29.4%) of the 490 results were multidisciplinary; 75 (15.3%) did not contain enough information to assign as multidisciplinary. When separating by region, an average of 24.8% of results were multidisciplinary with significant differences between regions noted (P = 0.003). The Mideast had the highest percentage (52.5%), whereas Alaska and Hawaii had the lowest (10%). For area types, no significant differences were found (P = 0.14) as 68 (26.5%) of metropolitan areas were multidisciplinary, whereas 76 (32.6%) of rural results were multidisciplinary; 51 (19.8%) of former and 24 (10.3%) of latter were unknown. However, when evaluating the clinics with multidisciplinary care by distance, similar disparities exist as significant differences are noted between metropolitan and rural areas (P Table 2).
Multidisciplinary Concussion Clinics Based on Area Type and Distance
| 51-100 Miles (n) | >101 Miles (n) | ||
| Metropolitan | 63 | 3 | 2 |
| Rural | 4 | 14 | 58 |
Significant differences seen between metropolitan and rural areas based on distance (P
Pediatric Trends
As noted, nationally, only 32.0% of the results saw pediatric patients, of which, 59 (37.6%) were also multidisciplinary. Some regions, such as Mideast (n = 9, 22.5%) and Southeast (n = 24, 20.0%), had 20% of their clinic sites both see pediatric patients and were multidisciplinary in nature. However, some regions, such as Alaska (n = 0), Hawaii (n = 0), Rocky Mountain (n = 0), and Southwest (n = 2, 4%), had less than 10% with both pediatric and multidisciplinary care.
Subspecialist Presence
Of the national totals (n = 490), the most common medical subspecialists present within clinics were sports medicine (n = 129, 26.3%), physical therapy (n = 199, 40.6%), & neurology (n = 114, 23.3%). Other multidisciplinary care teams included neuropsychology (n = 91, 18.6%), occupational therapy (n = 77, 15.7%), athletic training (n = 70, 14.3%), primary care (n = 69, 14.1%), physical medicine and rehabilitation (n = 69, 14.1%), surgical specialist (n = 65, 13.3%), and orthopedic surgery (n = 65, 13.3%); multiple areas had less than 10% including speech therapy (9.4%), alternative medicine (9.4%), emergency medicine (2.4%), radiology (0.2%), optometry (0.2%), and audiology (0.2%).
DISCUSSION
This study successfully applied a novel search strategy to evaluate geographic differences for pediatric patient populations when trying to access optimal care for management of mild traumatic brain injuries and concussions. The approach used was intended to mimic what families might do when searching their local region for specialty clinics. Nationwide, there is an overall lack of access to multidisciplinary concussion care for pediatric patients. Additionally, those in rural communities face more limitations related to access to facilities with increased distances from closest clinic sites.
Although nationally, 40% of sites were >50 miles away, this was a much higher differential for families in rural areas where nearly 80% were >50 miles away. This would be approximately 1 hour of travel in each direction for care; figures like this often do not account the cost to families for lost work time, lost school time, or other factors such as gas prices. The geographic constraints of access to health care can exacerbate existing healthcare disparities. Awareness of these differences in travel time can help to identify areas that might benefit from additional resources.13
Glaring gaps also existed for pediatric populations and multidisciplinary care. Less than 1/3 clinics were noted to be accessible to pediatric patients or offered multidisciplinary care. Of clinics that saw pediatric patients, the majority were not multidisciplinary. As per recommendations from the American Academy of Pediatrics, individualized management is critical for concussion care, often with need to use specialist support due to the risk of long-term symptoms and complications.14 Understanding how to best establish resources is imperative to reduce previously described disparities in youth concussion care, such as 1 single site study where patients seen in a specialized clinic were more likely to be White and have private insurance.15
This study highlights the need to establish resources to optimize concussion care based on newly identified gaps in access and optimal care features. The internet searches provide a way to look for resources that families might connect with locally. However, this study does have limitations. First, this study recognizes the continuing evolution of defining optimal concussion care for pediatric patients. The recently published consensus statement from the sixth International Conference on Concussion in Sport16 recommends both referral to clinicians with “specialised knowledge and skills in concussion management” and “a multimodal clinical assessment, ideally by a multidisciplinary team” for patient who are slow to recover, supporting the rationale for more access to specialty care. Although the features were analyzed based on the web site, information may not be updated or it may not reflect the actual abilities of sites to accept referral and perform services, such as seeing the full age range of pediatric patients. The study may not represent actual access to care as it may be obtained by care coordination through the primary care or by direct referral to a specialty clinic from the primary care team. Not all clinics provided an age range to define “pediatrics” so limitations may still exist for younger patients. In addition, this study does not fully address the availability and opportunity of telehealth to improve access to care; recognizing, though, that telehealth also has limitations regarding potential structural barriers with access to high-speed internet connections at affordable pricing.
In conclusion, this study highlights actions families may take to find concussion care locally. Disparities exist based on location, that is rural areas, with clinical gaps existing for the care of pediatric patients and in providing multidisciplinary care. The implication of these findings is that pediatric patients may have their concussion care negatively impacted due to the clinical gaps. Alternative means to provide expert care to areas of limited access should be explored, such as improved specialty training for rural health providers to coordinate concussion care and alternative care models using telehealth and remote patient monitoring to extend the reach of regional specialty clinics. Although the definition of optimal care is evolving, the findings of this study serve as the framework for medical centers and clinical providers to develop better projections of needs to establish access to quality concussion care for pediatric patients.
ACKNOWLEDGMENTS
The authors would like to thank Alexis Visotcky and Dr Ruta Brazauskas for their support on statistical analysis.
References
concussion management; pediatric; access to care; internet search