INTRODUCTION
The medial collateral ligament (MCL) is the most injured ligament in the knee.1–5 An MCL injury can be graded as mild, moderate, and severe, with laxity and valgus alignment increasing the severity of the grading. It is generally accepted that incomplete tears can be treated nonoperatively.6–8 However, there is no standardized treatment algorithm, given the complex anatomy of the medial knee and the common association with other structural damage.9,10 Nonoperative treatment of isolated MCL injuries avoids all the potential costs, risks, and complications resulting from surgery (eg, health care costs, infection, range of motion complications, longer recovery time).10,11 Combined MCL injuries involving the anterior cruciate ligament (ACL) are commonly studied.11–15 Most literature recommends nonsurgical management for the MCL using a range of motion (ROM) knee brace, followed by reconstruction of the ACL.7,10,11,16–19 Although nonoperative management yields good outcomes, some evidence indicates it may lead to more instability, lower functional scores, and a higher rate of osteoarthritis (OA).20,21
Nonetheless, treatment adherence is crucial for evaluating the effectiveness of nonsurgical management across all conditions.22 Adherence, rather than compliance, is a growing topic in health care as its value in successful treatment is more recognized.23–27 If a patient is compliant, they are acting according to a prescriber’s advice or directives. In modern medicine, the term may seem condescending to the patient.23,28 Conversely, adherence is defined by the World Health Organization as “the extent to which a person’s behaviour… corresponds with agreed recommendations from a health care provider”.29 The operational definition of adherence varies significantly within the literature.26,30,31 Some studies use an all-or-none approach (ie, adhering entirely or not at all) or “partially” or “completely” adherent.27,29,32 In contrast, others accommodate a range of adherence (ie, “always,” “often,” “sometimes,” “rarely,” and “never”).29,33 Measuring adherence can also be challenging. Within the physical rehabilitation literature, self-report logbooks are commonly supported.26,30,34–36
Patients may encounter difficulties in adhering to MCL bracing therapy because of the size of the brace, imposed mobility restrictions, and the necessity of wearing it continuously for up to 24 hours daily.37 Although numerous studies focus on adherence to physical rehabilitation postinjury, a few have investigated the determinants of treatment adherence,24,38–40 and none have examined adherence to knee brace wearing for MCL injuries. Examining brace wearing for MCL injuries is crucial to enable clinicians to anticipate the factors influencing adherence.41 This, in turn, helps patients overcome obstacles, leading to improved clinical outcomes.
The literature addressing MCL injuries treated with brace immobilization has suggested that the brace always needs to be worn.9,10,16,17,42,43 However, these studies are either based on animal models43 or do not adequately examine adherence.9,10,16,17,42 Therefore, the first objective of this study is to estimate adherence to the brace treatment among patients with isolated MCL or combined ACL–MCL injuries. The secondary aim is to examine the correlation between adherence and various patient and treatment factors, such as sex, age, body mass index (BMI), diagnosis, brace setting, affected knee, and days postinjury when braced. In addition, patient-reported outcomes, including pain, overall knee rating, and brace satisfaction, will be described for each 2-week phase within a 6-week MCL knee bracing treatment protocol.
METHODS
Study Design
This exploratory study was nested within a randomized clinical trial (RCT) examining the effectiveness of 2 different MCL bracing protocols at the sport medicine clinic (SMC).44 The SMC is an integrated academic and clinical facility that cares for patients from primary to tertiary levels. The acute knee injury clinic (AKIC) at the SMC defines complete tears of the MCL as moderate-to-severe isolated MCL or combined ACL–MCL injuries (Table 1). The acute knee injury clinic’s standard of care is to treat these injuries with 6 weeks of protection using a full-leg ROM-hinged knee brace.
Inclusion and Exclusion Criteria for the Randomized Clinical Trial
| Inclusion Criteria | Exclusion Criteria |
| • Age 18–65 yrs • Diagnosed with an acute isolated moderate or severe MCL sprain ≤2 wk old, or • Diagnosed with a combined MCL–ACL injury (ie, an ACL tear with an associated moderate or severe MCL sprain) ≤2 wk old • MCL injury is defined as: ○ Moderate MCL injury: ▪ Knee is stable with valgus stress testing at 0 degree extension ▪ Knee opens ≥2 mm ssd with valgus stress testing at 30 degrees flexion ○ Severe MCL injury, affected by alignment* ▪ Neutral/varus knee: • Knee opens ≥2 mm ssd with valgus stress testing at 0 degree extension • Knee opens ≥5 mm ssd with valgus stress testing at approximately 30 degrees flexion ▪ Obvious Valgus knee: • Knee stable with valgus stress testing at 0 degree extension • Knee opens ≥2 mm ssd with valgus stress testing at approximately 30 degrees flexion • Candidate for nonoperative management • Willing and able to follow-up for 12 wks postinjury |
• Operative management required within 12 wks postinjury • Previous ligament injuries to the injured and/or noninjured knee • Using/used one of the following braces before being seen in AKIC: ○ Knee immobilizer (eg, Zimmer brace) ○ Long-legged hinged brace (ROM or otherwise) • Unable to follow-up for 12 wks postinjury • Associated patellar dislocation • Knee dislocation • Locked knee • Combined MCL injury other than ACL/MCL (PCL, LCL, etc.) • Signs of radiologic OA, as defined by a grade C or D on the IKDC radiologic grading scale • Stiffness, defined as >20 degrees flexion contracture and/or |
IKDC, international knee documentation committee; LCL, lateral collateral ligament; PCL, posterior cruciate ligament; ssd, side to side difference.
Participants
Patients were recruited from the AKIC according to the inclusion and exclusion criteria given in Table 1. The AKIC nonphysician expert and sport medicine physicians performed a complete bilateral ligamentous knee examination following the standard AKIC practice.45 Patients with a confirmed acute isolated MCL or a combined ACL–MCL injury were screened for eligibility and presented with the study details. After a thorough informed consent process, participants were randomized to 1 of 2 range of motion settings: 0 to 90 degrees of flexion (Protected group) or 30 to 90 degrees of flexion (Restricted group). All patients were prescribed the same ROM-hinged knee brace (the Breg T-Scope Premier Post-Op Knee Brace (Breg Inc, Carlsbad, CA)).
All participants in the RCT who had undergone a minimum of 6 weeks of bracing treatment with sufficient daily adherence data were eligible and included in this bracing adherence study.
Measures and Definitions
Primary Outcome: Adherence
The treatment protocol included 3 distinct phases of 2-week increments. In phases 1 and 2, patients were required to wear their brace consistently except for daily personal hygiene (∼23 h/d). In phase 3, patients removed the brace at night, while maintaining consistent brace wearing during waking hours (∼15 h/d). Participants were asked to complete a daily adherence log. The log was emailed to the patient every morning at 10:00 am to report total nonbrace-wearing minutes from the previous day and the reason for brace removal. Two patient partners who had completed their participation in the RCT assisted with the definitions of adherence.46,47 A patient was a nonadherer if they were nonadherent (
Independent Variables
Patients were required to complete 2 questionnaires at the beginning of each phase (ie, baseline, 2, 4 weeks). The first was for patient-reported pain in their affected knee on a Visual Analogue Scale (VAS; 0–100, with 100 being the most pain possible). The second questionnaire reported their overall knee rating on the Single Assessment Numeric Evaluation (SANE; 0–100, with 100 being normal relative to their healthy knee).48,49 A higher SANE score is considered an indicator of healing.49 Pain and SANE were measured as continuous variables.
Patients were also given a modified patient satisfaction questionnaire (Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0) on a scale from 1 to 5, with 1 being “Not at all Satisfied” and 5 being “Very Satisfied”). The QUEST 2.0 included 8 questions about the patient’s satisfaction with various brace aspects (ie, ease of use, effectiveness, adjustability, durability, dimensions, weight, safety, and comfort). The brace satisfaction questionnaire was administered at the end of each phase (ie, 2, 4, 6 weeks) and was interpreted as an average score.50Table 2 outlines the bracing protocol and patient-reported outcomes timeline. All measures have been previously validated for use with similar populations and in comparable settings.48–50
Brace Treatment Protocol and Questionnaire Timeline
| Phase 1 (weeks 1–2) | Phase 2 (weeks 2–4) | Phase 3 (weeks 4–6) |
| Consistent brace wearing (∼23 h/d) | Consistent brace wearing (∼23 h/d) | Waking hours only (∼15 h/d) |
| Daily brace-wearing log @ day 1–14 | Daily brace-wearing log @ day 15–28 | Daily brace-wearing log @ day 29–42 |
| Pain (VAS) and overall knee rating (SANE) @ baseline | Pain and overall knee rating @ 2-wk visit | Pain and overall knee rating @ 4-wk visit |
| Brace satisfaction (QUEST 2.0) @ 2-wk visit | Brace satisfaction @ 4-wk visit | Brace satisfaction @ 6-wk visit |
Statistical Analysis
Data were analyzed using SPSS for PC, version 29.0.1.0. Data were explored numerically and graphically. Separate univariate logistic regression analyses were done to explore the predictability of patient characteristics (age, sex, diagnosis, BMI, affected knee, days postinjury when braced), brace group (0–90 degrees or 30–90 degrees), pain (VAS), overall knee score (SANE), and brace satisfaction (QUEST 2.0) on adherence for each of the 3 phases. Given the exploratory nature of this study, predictors identified in the literature and those with P-values
RESULTS
This study included all 60 patients in the RCT recruited between November 2020 and April 2023. One patient was excluded from the analysis because of insufficient adherence data. Sample demographics are described in Table 3.
Patient Characteristics for the Total Sample (n = 59)
| Patient Characteristics | |
| Sex, n (%) | |
| Male | 27 (46) |
| Female | 32 (54) |
| Age, μ (range) | 37.64 (19–65) |
| BMI, μ (SD) | 26.19 (4.92) |
| Days postinjury, μ (range) | 9.12 (2–18) |
| Affected knee, n (%) | |
| Left | 37 (63) |
| Right | 22 (37) |
| Brace group, n (%) | |
| Protected | 31 (53) |
| Restricted | 28 (47) |
| Diagnosis, n (%) | |
| MCL | 26 (44) |
| MCL–ACL | 33 (56) |
Adherence to the Bracing Protocol
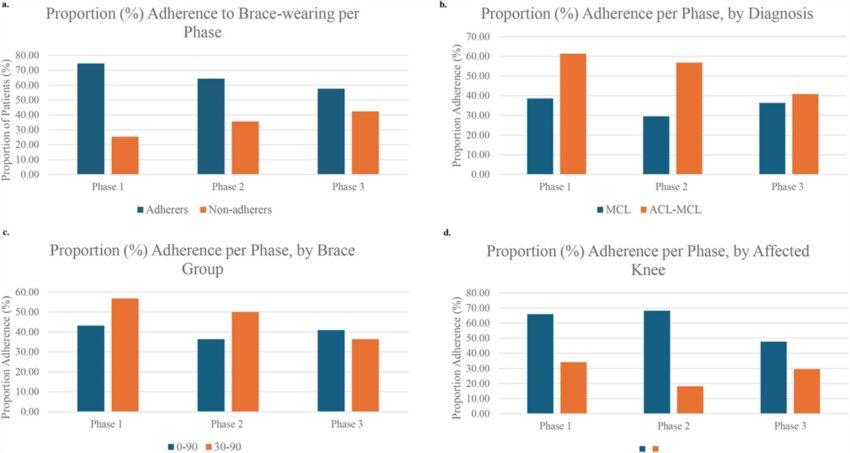
Adherence decreased over time (Figure 1A). In phase 1, 75% (44/59) of patients adhered to the protocol, 64% (38/59) in phase 2%, and 59% (35/59) in phase 3.
A, Proportion (%) adherence and nonadherence in each phase of the treatment protocol. B, Proportion adherence based on diagnosis (MCL or MCL–ACL) in each phase of the treatment protocol. C, Proportion adherence based on the assigned brace group (0–90 or 30–90) in each phase of the treatment protocol. D, Proportion adherence based on the affected knee (left or right) in each phase of the treatment protocol.
Those with a combined ACL–MCL injury seemed more adherent, particularly in phases 1 and 2 (Figure 1B). Those braced in the restricted brace group (30–90 degrees) reported higher brace-wearing adherence than the Protected (0–90 degrees) group in phases 1 and 2 (Figure 1C). Finally, patients with left-sided injuries were more adherent overall (Figure 1D).
Pain decreased over time, regardless of adherence or brace group. Figure 2A shows the change in pain scores from the start and end of each protocol phase, with a negative value representing a decrease in pain. Patients who adhered to either bracing protocol from baseline to 4 weeks (phases 1 and 2) had a more remarkable improvement in pain and reported minimal improvement in the third phase. Nonadherers demonstrated a slower recovery over time across all 3 phases.

A, Change in pain scores (on VAS) per phase of the protocol and adherence group. B, Overall knee ratings (SANE on VAS) per phase of the protocol and adherence group.
As illustrated in Figure 2B, SANE scores increased over the 3 phases of the protocol. There was no difference in SANE scores between groups in any phase. However, there was a trend that adherers reported greater improvement in SANE scores from baseline to the point of brace removal at 6 weeks. Patients classified as adherers rated their knee as 21.5% relative to their uninjured knee at baseline, which increased to 63.9% by the end of the treatment at 6 weeks. Similarly, nonadherers started higher at 29.1% and only increased to 56.7% by 6 weeks.
Overall brace satisfaction for the whole sample stayed relatively consistent throughout the 3 phases (phase 1: μ = 3.81, SD = 0.56; phase 2: μ = 3.73, SD = 0.59; phase 3: μ = 3.80, SD = 0.63). There were no statistical or clinically meaningful differences between adherers and nonadherers.
No noticeable trends existed between adherence and age, BMI, sex, and time since the injury when the brace was prescribed.
Factors Related to Adherence
The univariate analyses showed that brace satisfaction (phase 1), brace group (phases 1 and 2), pain (phases 1 and 2), and affected knee (phase 2) were associated with adherence. These variables were included in the exploratory multivariable logistic regression alongside those supported by the literature (ie, age and diagnosis). Table 4 details each predictor variable’s odds ratios and confidence intervals (CI) in the univariate and multivariable logistic regressions.
Odds Ratios and CI for Each Predictor Variable Included in the Univariate LR and the Multivariable LR in Each of the Treatment Protocol’s 3 Phases
| Phase 1 | Phase 2 | Phase 3 | ||||||||||
| Univariate LR | Multiple LR (P = 0.039)* | Univariate LR | Multiple LR (P | Univariate LR | Multiple LR (P = 0.775) | |||||||
| Exp (B) | 95% CI | Exp (B) | 95% CI | Exp (B) | 95% CI | Exp (B) | 95% CI | Exp (B) | 95% CI | Exp (B) | 95% CI | |
| Sex (ref group: female) | 0.730 | 0.22–2.401 | 1.512 | 0.518–4.416 | 0.667 | 0.234–1.896 | ||||||
| Age | 0.984 | 0.929–1.042 | 0.984 | 0.915–1.057 | 1.008 | 0.957–1.026 | 0.999 | 0.930–1.074 | 1.033 | 0.980–1.089 | 1.032 | 0.976–1.090 |
| BMI | 1.028 | 0.905–1.169 | 1.009 | 0.903–1.126 | 1.059 | 0.943–1.190 | ||||||
| Affected knee (ref group: left knee) | 1.692 | 0.514–5.564 | 4.085 | 0.602–27.721 |
7.500 (P |
2.267–24.812 |
4.924 (P = 0.054) |
0.975–24.878 | 0.909 | 0.312–2.650 | 1.048 | 0.304–3.612 |
| Diagnosis (ref group: MCL–ACL) | 0.800 | 0.243–2.633 | 0.244 | 0.033 | 2.286 | 0.771–6.777 | 1.576 | 0.322–7.715 | 0.750 | 0.264–2.134 | 0.607 | 0.174–2.120 |
| Brace group (ref group: 30–90 degrees) |
5.263 (P = 0.02) |
1.300–21.316 |
8.573 (P = 0.025) |
1.312–56.021 |
3.437 (P = 0.035) |
1.094–10.802 |
3.833 (P = 0.082) |
0.844–17.399 | 0.963 | 0.342–2.708 | 0.792 | 0.257–2.440 |
| Days postinjury | 1.115 | 0.953–1.303 | 1.020 | 0.894–1.164 | 1.004 | 0.884–1.140 | ||||||
| Pain (change score) |
0.972 (P = 0.089) |
0.941–1.004 | 0.981 | 0.942–1.002 |
1.068 (P |
1.028–1.109 |
1.066 (P = 0.006) |
1.018–1.116 | 1.000 | 0.972–1.029 | 1.001 | 0.971–1.003 |
| SANE | 0.986 | 0.961–1.012 | 0.993 | 0.966–1.021 | 1.008 | 0.982–1.035 | ||||||
| Brace satisfaction |
3.749 (P = 0.052) |
0.986–14.257 | 2.411 | 0.523–11.114 | 1.390 | 0.546–3.537 | 1.007 | 0.321–3.611 | 1.792 | 0.750–4.283 | 1.826 | 0.714–4.669 |
B, Exp; LR, logistic regression; OR, odds ratio.
*Indicates statistical significance (P
The multivariable logistic regression model for phase 1 demonstrated that being braced in the restricted bracing group significantly predicted adherence (P = 0.039). In phase 2, the regression model demonstrated that pain, having a left-sided injury, and being assigned to the restricted brace protocol were significant predictors of adherence (P P = 0.775).
DISCUSSION
This is the first study to explore factors that affect patient adherence to prescribed brace wearing after acute MCL injury of the knee. Patients with isolated and combined ACL–MCL injuries were included in an RCT comparing 2 bracing protocols: a Protected group (0–90 degrees knee flexion) and a Restricted group (30–90 degrees).
Overall, the descriptive analyses revealed that patient adherence to prescribed brace wearing decreased from 75% to 59% throughout the 3 phases of the study. Similarly, knee pain decreased over time, independent of diagnosis or assigned bracing group. Adherers reported a greater reduction in pain in phases 1 and 2. Patients’ knee ratings (SANE) improved over time. Brace satisfaction did not vary between groups or phases. There was no significant relationship between adherence and sex, age, BMI, days postinjury, or SANE scores.
The exploratory multivariable logistic regression model for phase 1 suggested that bracing in the restrictive setting (30–90 degrees) increased the likelihood of adhering by a factor of 8 (Table 4). The model for phase 2 suggested that pain reduction, being braced restrictively, and having a left-sided injury predicted adherence. Those braced restrictively were approximately 4 times more likely to be adherent, while the effect for those with left-sided injuries was nearly 5-fold (Table 4). The phase 3 model was not significant (Table 4). The variance in adherence explained by the model for phases 1 and 2 was moderate (phase 1: r2 = 0.326, phase 2: r2 = 0.526, phase 3: r2 = 0.076). Other factors likely affect adherence above and beyond what was examined in this exploratory study.
The finding that treatment adherence decreased over time is consistent with other studies examining nonoperative adherence to physiotherapy in patients with knee OA.27,38,51 The authors suggest that the decline in adherence may be related to disease severity, low self-efficacy, and symptom improvement.38 Similarly, adherence in this study may have decreased if the patients felt their symptoms had improved and received encouraging feedback from clinical staff regarding MCL recovery.27,30,52,53 Another explanation could stem from the gradual wear and tear of the brace, making it less comfortable or more challenging to wear over time. Nonetheless, satisfaction with the brace remained consistent throughout the study.
It is evident in the literature that patient-perceived pain influences adherence.38,54 If the treatment alleviates pain, patients are more inclined to adhere.38 In contrast, patients may be less adherent if the treatment does not improve their symptoms.30,38 In this study, pain and adherence were highest in phase 1, potentially suggesting that patients wore the brace to reduce pain.27 Once the pain improved, the need for bracing may have been less evident, resulting in reduced adherence. The increase in SANE knee rating scores over time reflects the same construct of symptom improvement. These findings may also suggest that patients recover over time regardless of adherence to the protocol.
There was no relationship between adherence and sex, age, or BMI throughout the 3 phases. This aligns with a 50-year review on patient adherence to medical recommendations, finding little evidence that gender affects adherence in adults.30 However, other related studies have shown an association between older age and improved adherence.55,56 The literature relating BMI to related treatment adherence is ambiguous.57–60
As demonstrated in phase 2, left-sided knee injuries were 8 times more likely to adhere to the bracing protocols. This may be because of the necessity of the right limb to drive a vehicle or be leg-dominant. Finally, this study indicated a relationship between adherence and diagnosis (isolated MCL or combined ACL–MCL) may exist. Those with a combined injury were likelier to adhere in all 3 phases. However, this was not statistically significant. Patients with more ligament damage may have worse symptoms and perceive a greater benefit from the brace.
Limitations
This study has limitations. First, it used a convenience sample from the RCT, which could have led to a selection bias.
Next, the adherence measurement tools used in the study relied on self-reported daily logs, which may be susceptible to recall bias and social desirability effects.25,40 To mitigate recall bias, patients received daily emails to complete the logs, which expired after 24 hours.25 Self-reporting also assumes patients are honest but may be influenced by social desirability.25,40 Techniques such as anonymity, independent questionnaire completion, and encouragement for honest responses were used to counteract this effect. Despite these challenges, self-report measures remain common and are not typically overinflated, according to recent reviews of adherence measurements.26,30,36
Next, there may have been other confounding or effect-modifying variables that influenced the relationship between adherence and the predictors. This study took a more exploratory approach to predicting adherence to MCL knee bracing. The sample came from a feasibility RCT. Therefore, the findings may be at risk for type II errors, and a larger sample size might yield more significant predictability of the models on adherence. Ultimately, the models accounted for 7.6% to 52.6% of the variance in adherence, suggesting that there may be other influential factors that were not measured.
This study could be generalized to patients treated nonoperatively for moderate-to-severe isolated MCL or combined ACL–MCL injuries. These findings would be generalizable to an active community practice where most patients participate in sports but may not relate to high-performance athletes.
Patients had regular clinical visits every 2 weeks, potentially with different sport medicine physicians. This may have led to variations in preferences in treatment that were inadvertently communicated to patients and affected their adherence throughout the treatment. Furthermore, patients tend to be more adherent if they have a good rapport with their clinician; thus, having different clinicians may have affected adherence.53,61 However, consistent interaction with a research assistant at each visit helped mitigate this. Finally, as RCT participants, they were likely more adherent than the general population, aided by daily adherence logs acting as reminders for brace wearing. Factors related to the clinical environment are challenging to quantify and necessitate a qualitative approach to understanding their impact on adherence.
Clinical Implications
Adherence to any treatment is usually associated with improved outcomes. Restricting knee range of motion from 30 to 90 degrees in a hinged knee brace has been shown to reduce laxity in the MCL at 3 months postinjury.44 Because little is known about adherence to knee bracing in patients with MCL sprains, this study has provided unique and valuable information. Clinicians may use these preliminary findings to inform their patients and prepare them for the intervention. First, bracing acute MCL injuries reduces pain over time and improves overall knee ratings, particularly during the first 4 weeks. Using a restricted bracing protocol may result in greater pain relief and improved outcomes with respect to knee stability.44 Second, it is more challenging for patients to use a brace on their right knee, likely because of concerns regarding driving safety and leg dominance. Finally, patients with combined ACL–MCL injuries are likely more adherent to their braces.
CONCLUSIONS
This study found that treatment adherence decreased over time among patients with MCL injuries. Pain also decreased, and overall knee scores improved. This exploratory study demonstrated several trends in improving adherence to knee bracing. Pain alleviation, restricting the range of motion of the brace, and having a left-sided knee injury significantly increased adherence in the first 4 weeks of treatment after injury.
ACKNOWLEDGMENTS
The authors thank the sport medicine physicians and nonphysician experts at the SMC and additional support from the Simpson Family Endowment.
References
treatment adherence; knee; acute injury; knee injury; knee bracing; nonoperative management; adherence; medial collateral ligament; compliance; sport medicine