INTRODUCTION
As described in the 2023 Amsterdam Consensus Statement on Concussion in Sport, a sport-related concussion (SRC) is “a traumatic brain injury caused by a direct blow to the head, neck, or body resulting in an impulsive force being transmitted to the brain” causing largely functional brain disturbances rather than structural injury.1 Although pathophysiology is complex, a proposed mechanism includes temporary disruption of ion channels involved in brain neurosignaling mechanisms, axonal injury, and changes to brain circulation. Signs and symptoms associated with a concussion may include but are not limited to somatic complaints, loss of consciousness, amnesia, balance impairment, behavior changes, cognitive impairment, and sleep/wake disturbance. Between 1.7 and 3 million sport-related and recreation-related concussions are diagnosed each year.2
Recent emphasis in public health has focused upon the danger of patients returning to contact athletic activity before concussion resolution. Individuals exposed to a second head impact before recovery from a previous concussion are at a greater risk for prolonged symptoms, more severe brain injury, or even death.3 Sports administrators at all competition levels strive to increase athlete safety by having medical personnel trained in concussion management evaluate injured athletes before they are allowed to return to play (RTP). According to the 2023 Consensus Statement, an evaluation should consist of medical assessments including a comprehensive history of the current injury, preinjury concussion risk factors, and detailed neurological examination assessing cognitive function, sleep/wake disturbance, ocular function, vestibular function, gait and balance, mood changes, and orthostatic symptoms.1,4
The diagnosis and management of concussion in the athletic population remains a clinical conundrum for physicians, juxtaposing the medical ethics of ensuring the best long-term outcome with the demand for accelerated RTP. Care providers are tasked with making an accurate assessment of a patient’s condition, providing counseling regarding recovery, and making RTP decisions that minimize athletes’ risk for long-term sequelae in time-constrained encounters. These difficult tasks are complicated by the lack of evidence-based standards in a field influenced by the lure of financial gains for multiple parties involved, further burdening the ethical health care provider.5
Multiple concussion assessment tools and clinical batteries exist to aid physicians in RTP decisions.6–8 These tools evaluate a variety of brain functions impacted by concussion, including cognitive processes, eye movement, hearing, balance, memory, mood, and exercise tolerance. With such a wealth of testing available, it can be difficult to choose which tests to use when making RTP decisions. Research regarding testing efficacy is challenging to analyze due to discrepancies in test administration and interpretation, individual patient characteristics, lack of validation, and absence of a gold standard in concussion diagnosis.9,10 Physicians are frequently confronted with incongruity between concussion assessment tools or inconsistent results within the same test, leading to uncertainty regarding an athlete’s safety in returning to play.11,12 There is also very limited provider feedback on the value of specific concussion assessments in the literature.
In this study, we surveyed members of the American Medical Society for Sports Medicine (AMSSM) to determine which concussion assessment tools they rely on when making RTP decisions. By analyzing the clinical experience of sports medicine physicians, practical knowledge of effective evaluation practices may be obtained and potential areas for improvement discovered.
METHODS
The Sanford Health Institutional Review Board and the AMSSM Research Committee approved this study (IRB# STUDY00002338). This is a cross-sectional, observational study using a web-based REDCap survey (Version 13.4.13). The survey was provided to the AMSSM Research Committee who distributed it to members through a secure email link. Participants clicked on a link on the survey’s first page to give their informed consent. Inclusion criteria encompassed being an active or fellowship member of the AMSSM who had graduated from residency and made an RTP decision for a patient after concussion in the last year. According to the AMSSM bylaws, active members must “(1) be licensed, practicing allopathic (M.D.) or osteopathic (D.O.) physicians (or the international equivalent), (2) be board certified in one or more of the Family Medicine, Internal Medicine, Pediatrics, Emergency Medicine, Physical Medicine or Rehabilitation specialties, and (3) have the required amount of points as specified on the Official Membership Application to qualify for active membership.” Fellowship members “must be board certified, licensed, practicing physicians of allopathic (M.D.) or osteopathic (D.O.) medicine who are engaged in a recognized Sports Medicine Fellowship Training Program.”13 At the time of survey distribution, associate and affiliate members were not included in the mailing list. Questions establishing inclusion criteria were presented in multiple-choice format. If a member had not made an RTP decision within the last year or had not yet completed residency, the survey immediately ended. The remainder of the survey consisted of demographic information describing a subject’s training and practice, lists of concussion assessments, and clinical scenarios. Answers were presented as buttons subjects clicked to signify their choices, and a text box was available if subjects wished to provide further explanation or record an answer not contained in the list. The survey is available as an electronic appendix (see Document, Supplemental Digital Content 1, https://links.lww.com/JSM/A483). Two reminder emails were sent during data collection, which extended from June to September 2021.
Descriptive statistics were calculated to identify concussion assessments in which sports medicine providers reported the most and least confidence. All analyses used SAS software, Version 9.4 of the SAS System for Windows 7 (PROC GLM) (Copyright © 2002-2012 SAS Institute Inc., Cary, NC). Descriptive analysis summarized the characteristics of the responses for various survey questions. χ2 tests for independence between demographic variables and outcome variables were performed in a univariate analysis. This study used a 95% confidence interval with an alpha level of 0.05.
Ethical Considerations
Participants experienced minimal risk from responding to this survey except for mild discomfort from recalling patient care. Responses were collected in a password-protected database, and only research staff had access to data. No identifying information was collected.
RESULTS
The study’s primary outcome is the normal concussion assessment that made physicians feel most confident a patient was ready to RTP. Secondary outcomes include assessments that made physicians feel least confident starting the RTP process, number and type of assessments performed by physicians, and variation in practice based upon demographic and training factors.
The survey was sent to 4552 AMSSM members. Based on 2020 AMSSM membership, 3099 were active, fellowship, or international members. Four hundred thirty members responded, and 392 met inclusion criteria, constituting a 12.6% response rate. Respondents were primarily male (279/392 (71%)). Approximately 38% (150/392) practiced sports medicine exclusively, and 66% (260/392) trained in family medicine as their primary specialty. Team physicians comprised 87.5% (343/392) of the respondents. Ninety-one percent (358/392) completed a sports medicine fellowship, 78.6% (308/392) had completed additional training in concussion, and 24.5% (96/392) had published research in the field (Table 1).
Demographic Characteristics of Survey Respondents
| Survey Respondents (n = 392) | AMSSM Demographic Data 2020 (n = 4392) | |
| Demographics | n (%) | % |
| Gender | ||
| Male | 279 (71.2) | 72 |
| Female | 105 (26.8) | 28 |
| Other | 8 (2.0) | — |
| Practice pattern | ||
| Primary specialty only | 4 (1.0) | |
| Mostly primary specialty | 57 (14.5) | |
| Equal primary/Sports medicine | 69 (17.6) | |
| Mostly sport medicine | 107 (27.3) | |
| Sports medicine only | 150 (38.3) | |
| Other | 5 (1.28) | |
| Years in practice since residency, mean (SD) | 11.99 (9.2) | |
| Team physician | ||
| Yes | 343 (87.5) | 79 |
| No | 49 (12.5) | 11 |
| At which level of competition are you a team physician?* | ||
| Olympic/paralympic/elite | 48 (12.2) | 14 |
| Professional | 97 (24.7) | 28 |
| Collegiate | 246 (62.8) | † |
| High school | 246 (62.8) | 67 |
| Youth | 74 (18.9) | 6 |
| Other | 7 (1.8) | |
| Primary specialty | ||
| Emergency medicine | 16 (4.1) | 4 |
| Family medicine | 260 (66.3) | 71 |
| Internal medicine | 28 (7.1) | 5 |
| Pediatrics | 49 (12.5) | 8 |
| Other | 11 (2.8) | 12‡ |
| Sports medicine fellowship | ||
| Yes | 358 (91.3) | |
| No | 34 (8.7) | |
| CAQ in sports medicine | ||
| Yes | 348 (88.8) | |
| No | 44 (11.2) | |
| Additional concussion training | ||
| Yes | 308 (78.6) | |
| No | 84 (21.4) | |
| Published concussion research | ||
| Yes | 96 (24.5) | |
| No | 296 (75.5) | |
| Gender treated | ||
| Female | 13 (3.3) | |
| Male | 38 (9.7) | |
| Equal number of all genders | 340 (86.7) | |
| Others | 1 (0.3) | |
*Because respondents could choose multiple options, percentages will not equal 100.
†The AMSSM categorizes collegiate team physicians into Division 1 (37%), Division 2 (12%), Division 3 (14%), NAIA (7%), and junior college (6%).
‡The AMSSM includes IM/Ped, physical medicine and rehabilitation, and other.
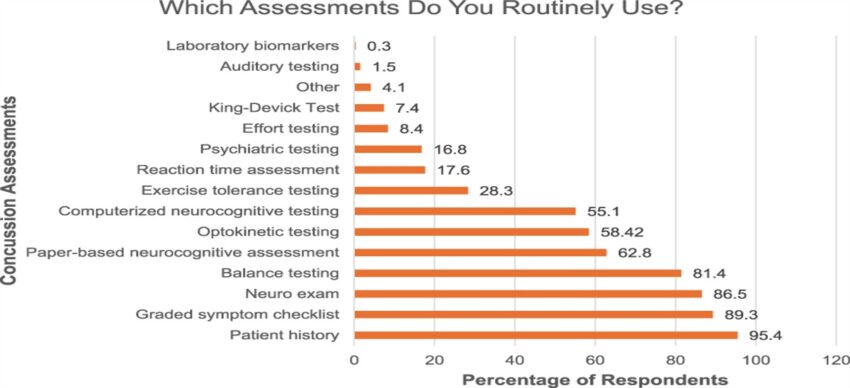
Subjects were asked which concussion assessments they routinely used when making RTP decisions. A majority of respondents included patient history, graded symptom checklist, neurological physical examination, balance testing, paper-based neurocognitive assessment, optokinetic testing, and computerized neurocognitive testing in their routine concussion evaluations. The most frequently used assessment was patient history at 95.4% (374/392) (Figure 1). Significant relationships between demographic factors and concussion assessments determined by χ2 test and Fisher exact test are outlined in Table 2.
Assessments used by sports medicine physicians for making RTP decisions for SRC.
χ2 Testing for Significant Relationships Between Physician Type and Concussion Assessments
| Physician Type | Assessment Routinely Included for Making RTP Decisions, n (%) |
P |
|
| Patient history | |||
| Yes | No | ||
| CAQ | 0.0227 | ||
| Yes | 39 (10.4) | 5 (27.8) | |
| No | 335 (89.6) | 13 (72.2) | |
| Exercise tolerance testing | |||
| Yes | No | ||
| Professional | |||
| Yes | 37 (33.3) | 60 (21.4) | 0.0133 |
| No | 74 (66.7) | 221 (78.7) | |
| Collegiate | |||
| Yes | 85 (76.6) | 161 (57.3) | 0.0004 |
| No | 26 (23.4) | 120 (42.7) | |
| Youth | |||
| Yes | 28 (25.2) | 46 (16.4) | 0.0435 |
| No | 83 (74.8) | 235 (83.6) | |
| Reaction time assessment | |||
| Yes | No | ||
| Collegiate | |||
| Yes | 52 (75.4) | 194 (60.1) | 0.0170 |
| No | 17 (24.6) | 129 (39.9) | |
| Youth | |||
| Yes | 19 (27.5) | 55 (17.0) | 0.0429 |
| No | 50 (72.5) | 268 (83.0) | |
| Optokinetic testing | |||
| Yes | No | ||
| Collegiate | 0.0012 | ||
| Yes | 159 (69.4) | 87 (53.4) | |
| No | 70 (30.6) | 76 (46.6) | |
| Balance testing | |||
| Yes | No | ||
| CAQ | 0.0170 | ||
| Yes | 30 (9.4) | 14 (19.2) | |
| No | 289 (90.6) | 59 (80.8) | |
| Computerized neurocognitive testing | |||
| Yes | No | ||
| Professional | 0.0442 | ||
| Yes | 62 (28.7) | 35 (19.9) | |
| No | 154 (71.3) | 141 (80.1) | |
| Collegiate | |||
| Yes | 158 (73.2) | 80 (50) | |
| No | 58 (26.9) | 88 (50) | |
| Graded symptom checklist | |||
| Yes | No | ||
| Collegiate | 0.0005 | ||
| Yes | 230 (65.7) | 16 (38.1) | |
| No | 120 (34.3) | 26 (61.9) | |
| CAQ | 0.0008* | ||
| Yes | 32 (9.1) | 12 (28.6) | |
| No | 318 (90.9) | 30 (71.4) | |
| Physician type | Reasons why the assessment is most useful, n (%) |
P value |
|
| I am contractually obligated to use it | |||
| Yes | No | ||
| Professional | 0.0145* | ||
| Yes | 4 (80) | 93 (24.0) | |
| No | 1 (20) | 294 (76.0) | |
| It has high-quality evidence for efficacy in the literature | |||
| Yes | No | ||
| Youth | 0.0370 | ||
| Yes | 24 (26.4) | 50 (16.6) | |
| No | 67 (73.6) | 251 (83.4) | |
| It most closely reflects resolution of the pathological processes behind concussion | |||
| Yes | No | ||
| High school | 0.0153 | ||
| Yes | 157 (67.7) | 89 (55.6) | |
| No | 75 (32.3) | 71 (44.4) | |
Subjects most often identified the graded symptom checklist as the most useful test for making RTP decisions (35.9% (135/392) of respondents) (Figure 2A). A follow-up question asked why they felt their chosen assessment was most useful, and most answered it closely reflected resolution of pathological processes underlying SRC (59.2% (232/392)) (Figure 2B).

A, and B, Responses for which concussion assessments are most useful for RTP decisions and why.
Subjects were then given clinical scenarios and asked to make RTP decisions based on SRC assessment findings. The first scenario asked which normal assessment made them feel most confident a patient’s concussion had resolved and it was safe to RTP. Approximately 30% (106/392) of respondents felt most confident starting the RTP process if the graded symptom checklist was normal (Figure 3A). The next scenario asked which abnormal assessment, in the context of all other normal assessments, they would most likely ignore and still allow RTP; the most common response was computerized neurocognitive testing (23.4% (84/392)) (Figure 3B). The last scenario asked which abnormal assessment, in the context of all other normal assessments, made them feel most concerned SRC had not resolved. The greatest percentage of physicians felt SRC had not resolved if the patient had an abnormal neurological examination (22.6% (81/392)), followed by optokinetic testing (20.1% (72/392)) and the graded symptom checklist (18.7% (67/392)) (Figure 3c). When given the opportunity to explain their answers in further detail, multiple respondents commented that it was very difficult to choose only 1 assessment for any of these measures and much depended upon the clinical circumstance.

A–C, Participants’ responses regarding the assessments that make them feel most and least confident about RTP and that they are most likely to ignore and allow RTP.
Ninety-seven percent (380/392) of physicians would wait to begin the RTP process if a patient had symptom resolution but all other concussion assessments were abnormal. Ninety-eight percent (384/392) would allow a patient with all normal assessments to RTP.
DISCUSSION
Our cohort of AMSSM members is composed of physicians acquainted with concussion management; nearly 79% completed additional concussion training outside of medical school, residency, or fellowship; almost 88% were team physicians; and about one-quarter had published concussion research. In addition, 91% completed a sports medicine fellowship, which is associated with performing a more thorough concussion evaluation than non–sports medicine fellowship-trained physicians.14 Examining their confidence in concussion assessment tools provides an understanding of the specialty’s practice patterns. The goal of the study was to identify concussion assessments in which physicians place their trust when making RTP decisions. Responses demonstrate a reliance on symptom reporting and an opportunity for clinical tool development.
The highest percentage of physicians reported a normal graded symptom checklist made them most confident starting the RTP process, although studies show symptom normalization does not consistently signal concussion resolution.15,16 Self-reported symptoms are subjective, and athletes may be motivated to underreport or omit symptoms to hasten RTP.17–19 Conversely, individual symptoms may be more reliable than total symptom scores and symptom severity scores at diagnosing concussion, even in the absence of a baseline.20 Efforts have been made to establish psychometric validity for tools commonly used in clinical practice, but the literature evaluating the psychometric properties of self-report scales is not exhaustive.21 Given the wide use of these scales, discontinuation would not be feasible, but clinicians should remain aware of their potential shortcomings.
Respondents named computerized neurocognitive testing as an abnormal assessment likely to be ignored when deciding to begin RTP; further research is necessary to investigate potential biases. However, abnormal tests such as the neurological examination and optokinetic testing made physicians feel less confident that SRC had resolved. This reveals that physicians view clinical tests as having positive or negative predictive values; although a normal optokinetic test does not necessarily correlate with SRC resolution, an abnormal examination is perceived as indicative of continuing concussion pathology. Data from such perceptions are used to calculate clinical predictive values and create clinical predictive rules. Le Sage et al22 developed a tool for predicting prolonged postconcussion symptoms from the emergency room, but a similar tool has yet to be formulated for RTP decisions in SRC. Sherry et al23 concluded that the total symptom inventory score and vestibular/oculomotor symptom provocation were the most sensitive and specific measures in a multimodal concussion assessment for diagnosing SRC, but similar knowledge is lacking regarding RTP assessments.
Concussion evaluation training in medical school and residency is limited, necessitating reliable tools to promote efficient, safe decision making. Canadian researchers found that the mean number of hours dedicated to category 1 learning about concussions in medical school was 2.65 hours, and the mean number of hours of category 2 learning was 7.5.24 Although this represents an increase in concussion education from previous years, further training is necessary to meet the recommended standards for concussion evaluation. Between 8% to 38% of US medical students reported receiving no teaching about concussion, and up to 24% did not remember being taught. Research on training is likewise limited because there have been no studies performed outside Canada quantifying time spent on concussion education in medical school.25,26
Most SRC examinations in practice are limited to 15 to 60 minutes, leaving the physician with little time for complicated data interpretation.27 This positions the graded symptom checklist as the most feasible, albeit incomplete, assessment on which to base RTP decisions. As the latest clinical guidelines recommend a multifaceted concussion evaluation, limiting assessments to 1 primary tool exposes physicians to legal liability and patients to increased risk. Although precise comparative statistics may vary, concussion treatment is generally associated with a higher rate of litigation due to increased public awareness and the potential for negative long-term outcomes.28 Evolution in clinical concussion assessment is required to meet the necessity for thorough evaluation in a reasonable encounter time.
Finally, numerous survey respondents remarked that it was very difficult to limit their answers to only 1 most or least useful assessment due to the complex nature of concussion presentation and management. This imposed difficulty was intentional on the part of the researchers to require subjects to make a decision given a complex presentation. Despite a wealth of clinical experience and tools available, survey respondents demonstrate that the RTP decision remains a balancing act. No tool has proven itself a single-assessment option, requiring the provider to integrate all available objective and subjective data and practice sound clinical judgment.27
Potential limitations of this study include confinement of subjects to AMSSM members only. Although the society includes the specialties of family medicine, pediatrics, internal medicine, emergency medicine, and physiatry, other disciplines involved in concussion management, such as neurology, orthopedic surgery, and physical therapy, were not represented. The demographic distribution of the specialties in our study differs from that of the AMSSM in that our study contains a higher percentage of pediatricians (12.5% compared with 8%) and lower percentage of family physicians (66.3% compared with 71%). Also, our study contains a greater percentage of team physicians (87.5%) than the AMSSM (79%). Other demographic factors are comparable (Table 1).29
Survey responses may not represent the concussion evaluation practices of all AMSSM members. Variability in the number of yearly concussion assessments conducted by study participants may introduce inconsistencies in data collection and affect reliability and generalizability. Because respondents were not required to answer all questions, provided multiple answers, and gave explanations in text boxes, the data sets have an unequal number of respondents; therefore, a multivariate analysis was not feasible and would violate power requirements for the study. Other limitations include the inability to evaluate all assessment tools. The survey used has not been validated in other studies, and it did not ask why physicians relied on some assessments more than others. For example, physicians reported less confidence in computerized neurocognitive testing, but it is unknown if this is because they lacked confidence in the test’s efficacy or their ability to perform and interpret it. Future directions may include a survey designed to perform multivariate analysis to better understand physicians’ motivations to favor certain assessments.
CONCLUSIONS
Concussion in sport remains a management challenge for medical providers. For members of the AMSSM, the normal assessment inspiring the most confidence for safe and successful RTP was the graded symptom checklist; the assessment instilling the least confidence for safe return was an abnormal neurological assessment. Subjects were most likely to ignore an abnormal computerized neurocognitive assessment and allow RTP if all other assessments were normal. These findings demonstrate clinical thought processes of concussion providers, reveal a reliance on symptom reporting, and showcase the potential benefit of decision tools and improved assessments for SRC.
ACKNOWLEDGMENTS
The authors thank the AMSSM Research Committee for their support in the creation and distribution of the survey. The authors also thank Dr Lisa MacFadden for her review of the manuscript.
References