INTRODUCTION
Adhesive capsulitis, commonly referred to as “frozen shoulder,” is a disabling and painful condition that affects approximately 2% to 5% of the general population,1 although estimates range up to 10%.2 The incidence is higher in female patients3 and individuals between the age of 40 and 65 years.4 While the etiology of primary adhesive capsulitis is largely unknown, numerous conditions have been associated with its development including diabetes mellitus,5 thyroid disorders,6,7 hyperlipidemia,8 autoimmune disorders,9 smoking,10 obesity,11 and low physical activity level.12 Shoulder trauma, surgery, and prolonged immobilization are each risk factors of secondary adhesive capsulitis.13
Adhesive capsulitis classically presents with shoulder pain and gradual loss of both active and passive range of motion (ROM). The natural history can be characterized by 3 distinct clinical stages.14 First, the “freezing phase” occurs with onset of shoulder pain and preserved ROM. Second, the “frozen phase” follows where pain may improve, but ROM is restricted, most notably shoulder external rotation. Finally, mobility gradually returns in the “thawing phase” with typical resolution over 3 phases ranging from 1 to 3 years. While it is often regarded as a self-limiting condition, incomplete restoration of ROM is common.15
The pathophysiology is thought to involve both inflammatory and fibrotic processes in the joint capsule, resulting in thickening of the adjacent synovial membrane, contracture of the capsule, and reduced capsular volume.14,16,17 Arthroscopic studies have demonstrated that the predominant site of pathology in adhesive capsulitis is at the anterior and axillary joint capsule, coracohumeral ligament, and the rotator interval.18–20 The rotator interval is located between the supraspinatus and subscapularis tendons. It is a triangular space that contains the anterosuperior portion of the glenohumeral capsule, superior glenohumeral ligament, coracohumeral ligament, and long head of the biceps tendon.21
Adhesive capsulitis is associated with significant pain and functional impairment. Initially, most patients with adhesive capsulitis are managed conservatively with steroid injections, medications, and physical therapy, although an evidence-based treatment algorithm has yet to be defined.22 A recent systematic review concluded that intra-articular corticosteroid injection may be superior to other nonsurgical treatments and further improvement results when combined with a home exercise program after injection.23 Moreover, steroid injection combined with hydrodilatation, which provides an immediate expansion of the capsule, may potentially expedite recovery.24
Glenohumeral joint steroid injections are commonly described using a posterior approach.25 However, some have suggested that an anterior injection approach targeting the rotator interval may allow for a more targeted and specific treatment based on the anatomy and observed pathology in adhesive capsulitis.26 Several randomized controlled trials (RCTs) comparing outcomes between the anterior and posterior approaches have yielded conflicting results.27–32 Therefore, the purpose of this systematic review and meta-analysis was to compare outcomes between the anterior and posterior glenohumeral injection approaches. The primary outcomes were pain visual analog scale (VAS) and shoulder ROM at 12 weeks, with secondary outcomes assessing patient-reported functional outcomes, accuracy, and adverse events. Given the current known pathophysiology of this condition, we hypothesized that the anterior approach would be associated with more pain reduction and increased ROM compared with the posterior approach.
METHODS
Systematic Review Registration
The protocol for this systematic review was registered at International Platform of Registered Systematic Review and Meta-Analysis Protocols (INPLASY202310080).
Search Strategy and Selection Criteria
We searched MEDLINE, Embase, Web of Science, and Cochrane Center Register of Controlled Trials for RCTs and prospective comparative studies that compared anterior and posterior glenohumeral joint approaches for steroid injection to treat adhesive capsulitis. The literature search was conducted per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and included all studies published from database inception through February 2023.33 A librarian affiliated with the authors’ institution was involved in building search terms (see Appendix A, Supplemental Digital Content, https://links.lww.com/JSM/A408). Reference lists of relevant articles were also used for a manual search. Randomized controlled trials or prospective comparative studies that compared outcomes between anterior and posterior approaches with steroids for adhesive capsulitis were eligible for inclusion.
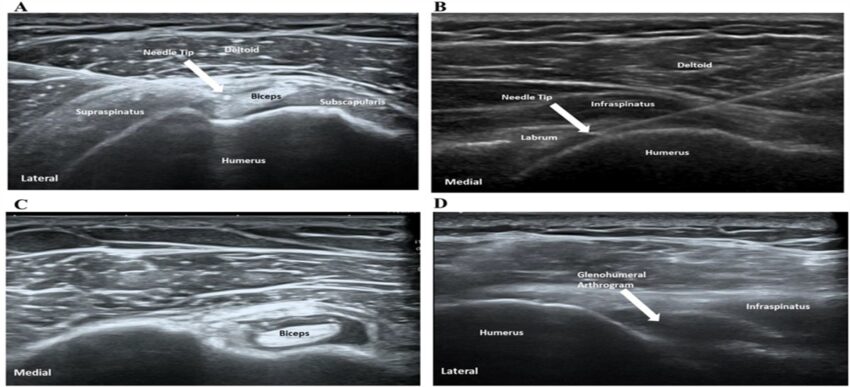
Briefly, the anterior approach was defined as an injection into the superior–anterior glenohumeral joint capsule. In the majority of studies included,27–29,31,32 needle placement was confirmed under ultrasound guidance, targeting just under the coracohumeral ligament either at the rotator interval or near the coracoid process (Figure 1A). Two articles30,34 used landmark-guided anterior glenohumeral joint injections, where the needle was inserted at the soft spot between the anterior acromion and coracoid, and advanced until contact with the humeral head was made. Posterior approach was defined as an injection into the glenohumeral space through the posterior deltoid (Figure 1B). In the ultrasound guided method, the space between the humeral head and glenoid labrum was visualized, and the injection was made into this space.27–29,31,32 In the landmark-guided posterior approach,30,34 the needle was inserted at the soft point, 2 to 3 cm inferomedial to the posterolateral acromion and advanced toward the coracoid process until contact with the humeral head was made. For the procedures, 21 to 23 gauge and 6-cm needles were used in the included studies.
Ultrasound-guided injection through the anterior rotator interval approach (A), posterior approach (B), postinjection extra-articular biceps tendon sheath flow (C), postinjection glenohumeral joint arthrogram (D). White arrows are pointing toward the injection target.
Articles written in English or in languages that could be translated to English were included. Studies in which anterior glenohumeral joint injections were combined with posterior/inferior glenohumeral joint injections, or extra-articular injections (subacromial bursa, biceps tendon, etc.) were excluded. Based on these criteria, 2 trials were excluded from our analyses because one study utilized 2 injections and targeted the coracohumeral ligament and inferior glenohumeral capsule,35 and the other study compared combined anterior and posterior injections and to the posterior approach alone.26 Furthermore, retrospective studies, case series, and case reports were excluded.
Data Extraction and Quality Assessment
Two authors independently evaluated each study from the initial search. Data extraction was independently conducted by 2 authors. Variables extracted from each article included country where the study was performed, study design, study inclusion/exclusion criteria, injection details (eg, ultrasound-guidance, hydrodilatation, dose, number of injections), rehabilitation protocols, follow-up periods, and adverse events. Patient characteristics including age, sex, laterality, arm dominance, and duration of symptoms were collected. The mean and SD of outcome measures after anterior and posterior shoulder injection were extracted for statistical analysis. When values were unavailable from the published manuscript, study corresponding authors were contacted for additional data. Two authors assessed the risk of bias with the revised Cochrane risk-of-bias tool for randomized trials for RCTs36 and the Newcastle–Ottawa Scale (NOS) for non-RCT.37 Discrepancies between 2 authors were resolved by discussion with a third author.
Outcome Measures
The primary outcomes of this meta-analysis were pain VAS and passive shoulder ROM (forward flexion, abduction, external rotation, and internal rotation) at 12 weeks. Secondary outcomes were pain VAS at 8 weeks, American Shoulder and Elbow scores (ASES) at 12 weeks, Constant–Murley shoulder score (Constant score), Shoulder Pain and Disability Index (SPADI) at 12 weeks, accuracy, and adverse events.
Statistical Analysis
We performed random-effects pairwise meta-analyses to account for clinical heterogeneity across the studies including patient and injection characteristics. Statistical heterogeneity was assessed with the Q and I2 statistics.38 The standardized mean difference (SMD) between anterior and posterior approaches was used as a measure of effect size for patient-reported outcomes including pain VAS, ASES, Constant score, and SPADI for better interpretability.39 Pain at rest was used for our meta-analysis.32 An SMD of 0.2 represented a small effect size, 0.5 represented a medium effect size, and 0.8 or larger represented a large effect size. For ROMs, the weighted mean difference (WMD) was used as a measure of effect size because the degrees of ROMs are directly interpretable. For accuracy, a meta-analysis of proportion was conducted. Subgroup analyses were performed with studies that used corticosteroids without hydrodilatation and studies that used ultrasound-guidance for injections. Publication bias was not assessed because the included number of studies was less than 10. STATA Version 16 (StataCorp, LLC, College Station, TX) was used for all analyses.
RESULTS
Eligible Studies and Characteristics of Included Studies
The initial search of published articles yielded 1066 studies. Three hundred sixty duplicate articles were removed. Of 706 articles reviewed, 676 articles met exclusion criteria based on review of titles and abstracts. Thirty studies were reviewed in full, and 23 studies were excluded based on ineligible intervention, study design, comparator, or patient population. The resulting 7 articles identified in the search were included in the meta-analysis. The review process is outlined in the PRISMA flow diagram (Figure 2).

PRISMA (preferred reporting items for systematic meta-analyses) diagram showing selection of articles for this meta-analysis.
Of the studies included, 6 were RCTs, and one study was a sequential prospective cohort study. Together, the studies comprised 468 patients, of which 241 patients received anterior injections, and 227 patients received posterior glenohumeral joint injections. The sample sizes of specific studies ranged from 23 to 54 patients in either the anterior or posterior injection group. The majority of patients were in their 50s, and most patients were female (n = 60%). Inclusion criteria for all studies required that patients have a primary diagnosis of adhesive capsulitis without secondary causes of shoulder pain based on clinical findings, imaging, or both. In addition, 5 studies had criteria for duration of shoulder pain ranging from more than one month to more than 9 months. Patients received ultrasound guided injections in 5 studies.27–29,31,32 In all 7 studies, patients received one injection containing between 3 and 20 mL of injectate comprised corticosteroid (40 mg triamcinolone in 5 studies or 40 mg methylprednisolone in 2 studies), lidocaine, normal saline and/or contrast. Three studies utilized hydrodilatation along with steroid injections when comparing the 2 approaches.28,29,32 Hydrodilatation was performed for both the anterior and posterior approaches in these 3 studies.
Following the injection, 5 studies provided patients with home exercise regimens, one study provided patients with physical therapy–guided exercises, and one study did not report a rehabilitation program. Patients were followed for 12 weeks after injection at various intervals.
Further characteristics of individual studies are summarized in Table 1.
Summary of Individual Study Characteristics
| Study | Year | Country | Study Design | Inclusion Criteria | Anterior Injection | Posterior Injection | Ultrasound | Hydrodilatation | Injection | Rehabilitation | Outcome Measures | Follow-Up | Adverse Events | ||||
| Patients (n, Mean Age, yr ± SD) | Female (%) | BMI (Mean ± SD) | Patients (n, Mean Age, yr ± SD) | Female (%) | BMI (Mean ± SD) | ||||||||||||
| Cho et al27 | 2022 | South Korea | RCT | 1) Shoulder pain with limitation of passive motion of >30° in 2 or more movement planes at the time of presentation 2) Plain radiography and magnetic resonance imaging to rule out secondary causes of painful stiffness |
43, 54.1 ± 8.9 | 41.9 | 23.6 ± 3.0 | 45, 55.4 ± 9.9 | 55.6 | 23.7 ± 2.6 | Yes | No | 1 mL (40 mg/mL) triamcinolone acetonide, 3 mL 1% lidocaine, 3 mL of water-soluble unionized contrast, 3 mL of normal saline (total volume: 10 mL) | Home-based exercise program with pendulum exercises, wall-climbing exercises, and gentle ROM exercises using a bar (3 times/day, 15 minutes/round). Patients were asked to refrain from provoking postmobilization soreness with self-feedback | Primary: Pain VAS score, ASES score, SSV, passive ROMs | 3, 6, and 12 wk | No patients reported serious adverse effects |
| Deng et al30 | 2023 | China | RCT | 1) Age older than 18 years with unilateral shoulder pain and limited movement diagnosed with primary frozen shoulder 2) Duration of pain >9 months and VAS score >3 3) Limitation of active and passive movement of the affected shoulder joint by > 30° relative to the contralateral shoulder joint in at least 2 movement planes 4) Routine shoulder x-ray and/or MRI to exclude other pathologies |
30, 54.5 ± 5.7 | 76.7 | 23.8 ± 2.5 | 30, 55.3 ± 3.9 | 66.7 | 24.5 ± 2.5 | No | No | 1 mL (40 mg/mL) triamcinolone acetonide, 4 mL 2% lidocaine (total volume: 5 mL) | Self-exercise program composed of flexion, abduction, external rotation and internal rotation under mild active training, and each exercise was performed 15-20 times during a period (3 times/d, 15 min/period). Patients were excluded if the exercise was not strictly performed during the 12-wk follow-up period | Primary: Pain VAS, constant–Murley shoulder score Secondary: Passive ROM and complication |
4, 8 and 12 wk | One patient in the anterior injection group experienced temporary symptoms associated with needle syncope |
| Elnady et al28 | 2020 | Egypt | RCT | 1) Age 35 to 60 yrs 2) Pain and stiffness in only one shoulder, for 1 to 6 mo 3) Restriction of passive motion, as measured with goniometer |
32, 45.4 ± 4.9 | 75.0 | — | 32, 47.6 ± 13.5 | 71.9 | — | Yes | Yes | 1 mL (40 mg/mL) methyl-prednisolone acetate, 1 mL 2% lidocaine, 15 mL normal saline (total volume: 17 mL) |
Physiotherapist-guided stretching and strengthening exercise program, every other day for 12-wk follow-up period | Primary: Pain VAS, SPADI | 12 wk | Seven patients (3 with posterior approach and 4 with anterior approach) experienced transient local pain and facial flushing following injection. Three patients (2 with posterior approach and 1 with anterior approach) required pain relief with NSAIDs for 72 h following injection |
| Kim et al29 | 2017 | South Korea | RCT | 1) Shoulder pain and limitations of active and passive motion in at least 2 directions on the initial checkup 2) MRI or ultrasonography with no secondary cause for adhesive capsulitis |
23, 55.5 ± 11.1 | 56.5 | — | 23, 52.8 ± 7.6 | 69.6 | — | Yes | Yes | 1 mL (40 mg/mL) triamcinolone, 4 mL lidocaine, 4 mL normal saline, 3 mL omnipaque (total volume: 13 mL) | Stick exercises started at 3 wks, and TheraBand exercises started at 7 wks after injection | Primary: Pain VAS, ROM, SAT, ASES, constant–Murley shoulder score Secondary: Consumed time |
3, 7, and 13 wk | Not reported |
| Rijs et al34 | 2021 | Netherlands | S-PCT | 1) Clinical symptoms 2) Shoulder pain with impaired passive glenohumeral ROM of ≥30° in 2 or more planes 3) Radiographs and ultrasound or MRI to confirm diagnosis and rule out other causes of shoulder pain |
54, 54.0 ± 4.0 | 63.0 | 23.0 ± 3.0 | 41, 52.0 ± 5.0 | 58.5 | 24.0 ± 3.0 | No | No | 1 mL (40 mg/mL) methylprednisolone, 2 mL (10 mg/mL) lidocaine, 3 mL (320 mg L/mL) loxaglic acid (total volume: 6 mL) | Not reported | Primary: Accuracy of the injection (contrast fluid localized in the glenohumeral joint without leakage of contrast fluid in the soft tissue or subacromial space) | N/A | Not reported |
| Sun et al25 | 2017 | China | RCT | 1) Age 18 to 70 yrs 2) Primary frozen shoulder 3) Normal radiograph finding of the affected shoulder 4) Loss of passive motion of the glenohumeral joint >25% or 30° in at least 2 planes when compared with the contralateral side or normal value 5) Pain VAS >7 6) Duration of symptoms |
27, 52.6 ± 4.4 | 59.3 | — | 24, 55.1 ± 3.4 | 58.3 | — | Yes | No | 1 mL (40 mg/mL) triamcinolone, 2 mL 2% lidocaine (total volume: 3 mL) | Home regimen of daily shoulder exercises | Primary: Pain VAS Secondary: Constant score, (DASH core, passive ROM) |
4, 8, and 12 wk | One patient in each group experienced temporary facial flushing following injection |
| Wang et al8 | 2021 | Taiwan | RCT | 1) Age 35 to 65 yrs 2) Duration of symptoms >1 mo 3) Limitation in the passive ROM >30° when compared with the contralateral side in at least 2 of these movements: forward flexion, abduction, or external rotation |
32, 52.4 ± 6.4 | 62.5 | 22.9 ± 3.8 | 32, 54.0 ± 7.0 | 59.4 | 24.1 ± 3.1 | Yes | Yes | 4 mL (10 mg/mL) triamcinolone acetonide, 4 mL 2% lidocaine hydrochloride, 12 mL normal saline (total volume: 20 mL) | Home exercise program consisted of Codman exercise, wall-climbing exercise, shoulder external and internal rotation exercise using the bar, and towel stretching exercise behind the back. All patients started the exercises at the first day after injections (at least 2 times/d) Patients were also allowed to receive physical therapy with hot packs, ultrasound diathermy, and inferential current therapy at specific outpatient clinics |
Primary: SPADI score Secondary: Pain VAS, ROM of the shoulder |
6 and 12 wk | One patient in each group endorsed severe pain (VAS > 4) following injection that spontaneously resolved without additional intervention |
DASH, disability of arm, hand, and shoulder; PC, posterior capsule approach; RI, rotator interval approach; SAT, patient satisfaction; S-PCT, sequential prospective comparative study; SSV, subjective shoulder value.
Study Quality and Risk of Bias Assessment
Figure 3 displays overall risk of bias assessment of included RCTs. All RCTs used randomized allocation sequence of patients with no baseline difference between groups. Patients in all studies were aware of their assignment as patient positioning during the procedure differs according to the injection approaches. However, there were no deviations from the interventions because patients in the included studies underwent rehabilitation as planned following their procedures. Outcomes were available for nearly all randomized patients throughout the studies except for those who dropped out. In the end, among the 6 included RCTs, 4 studies were judged to have a low risk of bias.27–29,32 One study30 was judged as having a high risk for bias because ASES, which was listed as a primary outcome, was not reported. A separate study did not provide clinical trial registration information, and therefore, we could not assess risk of selection bias.31 The only prospective comparative study was judged to have a low risk of bias.34

Risk of bias assessment for randomized controlled trials included in this meta-analysis.
Pain Visual Analog Scale
In all 6 RCTs27–32 included in our meta-analysis reported significant improvement in pain at 12 weeks following interventions with both anterior and posterior approaches. A meta-analysis of these 6 RCTs demonstrated that there was no significant difference in pain VAS at 12 weeks between 2 approaches (Figure 4A, SMD, −0.86; 95% CI, −1.76 to 0.04; I2, 93.8%).
Meta-analyses of randomized controlled trials comparing the anterior and posterior approaches at 12 weeks. A, Pain visual analog scale, (B) flexion, (C) abduction, (D) external rotation, (E) internal rotation. CI, confidence interval; SMD, standardized mean difference; WMD, weighted mean difference.


Range of Motion
A meta-analysis of 6 RCTs27–32 demonstrated a greater improvement of external rotation with anterior approach (Figure 4B, WMD, 8.08; 95% CI, 0.79-15.38; I2, 88.5%). A meta-analysis of 5 RCTs27,28,30–32 showed a significant difference between the 2 approaches in shoulder abduction at 12 weeks favoring the anterior approach (Figure 4C, WMD, 6.76; 95% CI, 3.05-10.48; I2, 0.0%). However, there were no significant differences in forward flexion (Figure 4D, WMD, 5.86; 95% CI, −0.12 to 11.84; I2 72.5%)27–32 and internal rotation (Figure 4E, SMD, −0.11; 95% CI, −0.35 to 0.13; I2, 14.6%).27–30,32
Secondary Outcomes
A meta-analysis of 2 RCTs30,31 that had data available for pain VAS at 8 weeks showed that there was no significant difference between 2 approaches (see Appendix Figure A, Supplemental Digital Content, https://links.lww.com/JSM/A409, SMD, −2.32; 95% CI, −4.68 to 0.03; I2, 95.1%). A meta-analysis of 2 RCTs27,29 demonstrated that there was no significant difference in ASES at 12 weeks between the 2 approaches (see Appendix Figure B, Supplemental Digital Content, https://links.lww.com/JSM/A410, SMD, −0.26; 95% CI, −0.81 to 0.28; I2, 57.0%) A meta-analysis of 3 RCTs29–31 showed that there was no significant difference in Constant scores at 12 weeks between the 2 approaches (see Appendix Figure C, Supplemental Digital Content, https://links.lww.com/JSM/A411, SMD, 0.98; 95% CI, −0.76 to 2.71; I2, 95.7%). A meta-analysis of 2 RCTs demonstrated that there was no significant difference in SPADI at 12 weeks between the 2 approaches (see Appendix Figure D, Supplemental Digital Content, https://links.lww.com/JSM/A412, SMD, −0.96; 95% CI, −2.77 to 0.84; I2, 95.3%).
Subgroup Analyses
A meta-analysis of 2 RCTs28,32 evaluating steroid injection with hydrodilatation demonstrated a significant difference in pain VAS at 12 weeks favoring the anterior rotator interval approach (see Appendix Figure E, Supplemental Digital Content, https://links.lww.com/JSM/A413, SMD, −0.52; 95% CI, −0.98 to −0.07; I2, 38.1%). A meta-analysis of 4 RCTs27,29–31 investigating a single injection of steroid without hydrodilatation showed that there was no significant difference between the 2 approaches in pain VAS at 12 weeks (see Appendix Figure E, Supplemental Digital Content, https://links.lww.com/JSM/A413, SMD, −1.08; 95% CI, −2.57 to 0.41, I2, 96.2%). Furthermore, a meta-analysis of 5 studies that utilized ultrasound-guidance for injection demonstrated that there was no significant difference in pain VAS between the 2 approaches at 12 weeks (SMD, −0.88; 95% CI, −1.97 to 0.22; I2, 94.8%).
Accuracy
Three studies27,29,34 reported the accuracy of injections with an overall pooled estimate of 87% (95% CI, 76%-98%; I2, 68.8%) for the anterior approach and 87% (95% CI, 78%-97%; I2, 35.6%) for the posterior glenohumeral joint approach.
Adverse Events
The procedures were well tolerated in both approaches without major complications throughout the studies (Table 1). Minor adverse events included transient local pain, perspiration, and facial flushing.
DISCUSSION
This meta-analysis compared outcomes between anterior and posterior glenohumeral joint steroid injections for the treatment of adhesive capsulitis. Based on the available RCTs, the anterior approach resulted in greater improvements in shoulder external rotation and abduction at 12 weeks. While there was no significant difference between the 2 approaches in patient-reported pain and functional outcomes at 12 weeks, subgroup analyses identified that the anterior approach may offer further benefit when steroid injection is combined with hydrodilatation. Both injection approaches had similar accuracy and were tolerated well without major complications.
Patient-Reported Pain and Function
The onset of adhesive capsulitis is associated with an inflammatory hypervascular synovitis, which gradually leads to abnormal fibroblastic proliferation in the adjacent joint capsule.40 Moreover, in patients with adhesive capsulitis, synovial tissue has been found to have increased expression of inflammatory cytokines.20 Treatment with an intra-articular steroid injection is intended to control pain by reducing inflammation and prevent progression of capsular fibrosis. Several systematic reviews with meta-analyses have reported that intra-articular steroid injections are effective in patients with adhesive capsulitis for relieving pain, improving functional performance, and increasing ROMs.23,25 Our meta-analysis expands on these findings to suggest that both anterior and posterior glenohumeral joint approaches for intra-articular steroid injections are effective at reducing pain 12 weeks. In addition, when hydrodilatation is performed along with steroid injection, the anterior approach may provide greater pain reduction at 12 weeks. Since the primary pathologic sites in adhesive capsulitis are thought to involve the rotator interval, anterior/axillary joint capsule, and coracohumeral ligament,40–42 the anterior approach, directly targeting some of these structures might have contributed to more pain reduction than the posterior approach. This theory is supported by a recent RCT (excluded from the present review) that demonstrated greater improvements in VAS and shoulder ROM (in abduction, external rotation and internal rotation) when patients received combined injections to the rotator interval and inferior glenohumeral capsule compared with posterior glenohumeral joint injections.35 Previous studies have also demonstrated benefit from subacromial–subdeltoid bursa injection in patients with adhesive capsulitis.31,43 It is therefore possible that steroid injection into the anterior rotator interval, especially with hydrodilatation, may result in greater improvements in pain due to the spread of medication into the adjacent subacromial–subdeltoid bursa.
Range of Motion
Given the progressive nature of adhesive capsulitis, it is crucial to preserve ROM in the early stage of disease. Usually, the coracohumeral ligament is the first structure to be affected. Thickening and shortening of this ligament, which forms the roof of the rotator interval,44 can result in restriction of external rotation.45,46 Furthermore, thickening and contracture of the rotator interval capsule and ligamentous structures may lead to multidirectional limitation of shoulder motion as demonstrated in a cadaveric study which found that sectioning of these structures improved passive ROM in flexion, extension, external rotation, and adduction.47 Given these observations, the anterior approach has been postulated to offer greater improvements in ROM. The results of our meta-analysis partially support this hypothesis given greater improvements in external rotation and abduction with the anterior approach.
Restriction in internal rotation, on the other hand, is thought to be limited by both anterior structures (coracohumeral ligament)48 and posterior structures (posterior capsule tightness).49,50 This may explain why there was no significant difference between the 2 approaches with internal rotation. Further studies are needed to elucidate mechanisms on how different injection techniques selectively affect specific ROM measurements.
Accuracy
Targeting the rotator interval may be more technically challenging than the posterior glenohumeral joint due to its smaller space and volume.51,52 Moreover, a previous cadaver study showed that the anatomy of the rotator interval can vary among patients,44 which may explain lower accuracy of the anterior injection in one study27 included in our meta-analysis. Interestingly, the accuracy of the anterior approach was significantly higher using anatomic landmarks compared with the posterior approach in another study included in our meta-analysis.34 These conflicting results may suggest that the accuracy may be operator dependent. Our meta-analysis of 3 studies27,29,34 showed that accuracy for both anterior and posterior approaches was 87% with overlapping confidence intervals. Similar accuracy between the 2 approaches may also suggest that there may be pathologic structures which are preferentially targeted through the anterior approach compared with the posterior approach. Future trials are warranted to investigate whether accuracy is associated with clinical outcomes, if there is a difference in accuracy using ultrasound and anatomic landmark guidance, and if there is a difference in accuracy between experienced and inexperienced operators.
Clinical Implication
Our meta-analysis supports the utilization of either anterior or posterior glenohumeral joint steroid injections in the treatment of adhesive capsulitis for pain control. However, the anterior approach may be more beneficial in restoring shoulder external rotation and abduction. The subgroup analysis also revealed that when combining steroid injection and hydrodilatation, the anterior rotator interval approach may offer greater pain reduction than the posterior approach. Based on the included studies, there was no major adverse event reported with either approach. Other potential benefits of the anterior approach include better visualization through rotator interval than posterior glenohumeral recess (especially in obese patients), as well as the ability to monitor facial expressions of pain or discomfort with the anterior approach.28,53 Positioning time was also significantly faster with the anterior approach.29
Limitations
This study has several limitations. First, steroid type and doses as well as rehabilitation protocols following injections were not uniform across the studies. However, we performed random-effects meta-analyses and subgroup analyses to address such heterogeneity. Additional studies assessing higher steroid volume may be necessary given that none of the included studies used more than 40 mg of triamcinolone or methylprednisolone. Second, the results of several secondary outcomes or subgroup analyses derived from only 2 studies, reflecting the need for future trials to substantiate these findings. Third, most studies included in our analysis were published in Asian countries, including South Korea, China, and Taiwan (n = 5). It is unknown whether the results of this meta-analysis may be generalizable to other populations. Finally, the follow-up times of the included studies were limited to 12 weeks. Owing to the progressive nature of adhesive capsulitis, further studies are needed to assess if there is any difference between the anterior and posterior approaches during long-term follow-ups, at least 6 months, if not one year, or following multiple injections.
CONCLUSIONS
There was no significant difference in terms of pain control between the anterior approach and posterior glenohumeral joint approaches. However, the anterior approach may be more beneficial in restoring shoulder external rotation and abduction at 12 weeks. In addition, steroid injection combined with hydrodilatation may offer greater pain reduction when performed with the anterior rotator interval approach at 12 weeks.
ACKNOWLEDGMENTS
The authors thank Anne Fladger at Countway library, Harvard Medical School for helping us with building search terms and identifying relevant studies for this review.
References