INTRODUCTION
Plantar fasciopathy is the most common cause of plantar heel pain, affecting approximately 10% of the US population.1,2 It most often affects patients in their fifth and sixth decades of life.3,4 Current options for initial and conservative treatments include oral nonsteroidal anti-inflammatory drugs, physical therapy, corticosteroid injections, platelet-rich plasma injections, splinting, and bracing.1,4–6 Historically, patients with symptoms refractory to conservative treatments were left with operative intervention as their only option.1
For patients with persistent symptoms, an ultrasonic fasciotomy offers a minimally invasive treatment option before consideration of surgical intervention. The procedure is performed with local and/or regional anesthesia and requires a small 3-mm incision. Under ultrasound (US) guidance, the device is guided to the region of pathology and using ultrasonic energy, pathologic tissue is debrided and removed while healthy tissue is preserved. The minimally invasive nature of this procedure offers several potential benefits, including reduced postoperative pain, faster recovery times, and fewer complications compared with traditional open surgery.
Although most of the existing literature on ultrasonic fasciotomy for plantar fasciopathy is limited to case reports, case series, and small prospective studies, the results are promising. A study by Higginson et al7 demonstrated that 92% of patients reported minimal to no pain in their heel at 12- to 18-month postprocedure follow-up, with 94% of patients feeling “very satisfied” or “satisfied” with their outcomes. Furthermore, Razdan and Vanderwoude8 showed that in 65 patients treated with an ultrasonic fasciotomy, there was a statistically significant improvement in Foot and Ankle Disability Index scores at 2 weeks post-procedure, and this significant improvement was sustained at 6 weeks.
The primary aim of our study was to prospectively evaluate the efficacy of an ultrasonic fasciotomy for chronic plantar fasciopathy and patients’ reported satisfaction with the procedure. We hypothesized that an ultrasonic fasciotomy for chronic plantar fasciopathy would be a safe and effective treatment of plantar fasciopathy, with continued symptom improvement and high patient satisfaction up to 1 year post-procedure. To the best of our knowledge, this is the largest review currently in the literature.
METHODS
Study Design
This prospective observational study included patients seen in our sports medicine clinic who underwent an ultrasonic fasciotomy procedure for the treatment of chronic plantar fasciopathy. All patients were evaluated, diagnosed, and treated by the primary author (R.C.K.), who at the time had 4 years of experience independently performing diagnostic US and US-guided microsurgical procedures, including 310 plantar fascia ultrasonic fasciotomies. The study was approved by our local institutional review board.
Patients
Patients with a diagnosis of chronic plantar fasciopathy who underwent an ultrasonic fasciotomy between January 2020 and March 2023 were included. Inclusion criteria included (1) age 18 to 80 years, (2) chronic plantar hindfoot pain for greater than 3 months duration, (3) failure of at least 6 weeks of conservative treatments, and (4) sonographic findings consistent with plantar fasciopathy. Exclusion criteria included (1) age range outside of 18 to 80 years, (2) chronic opioid use for greater than 3 months, and (3) non-English speaking.
Equipment
Diagnostic US examinations of the plantar hindfoot were performed using the Canon Aplio i800 machine and a 14-MHz high-frequency linear array transducer (Canon Medical Systems USA, Inc, Tustin, CA). The ultrasonic fasciotomies were performed using a TX2 device (Tenex Health, Lake Forest, CA).
Procedure Specifics
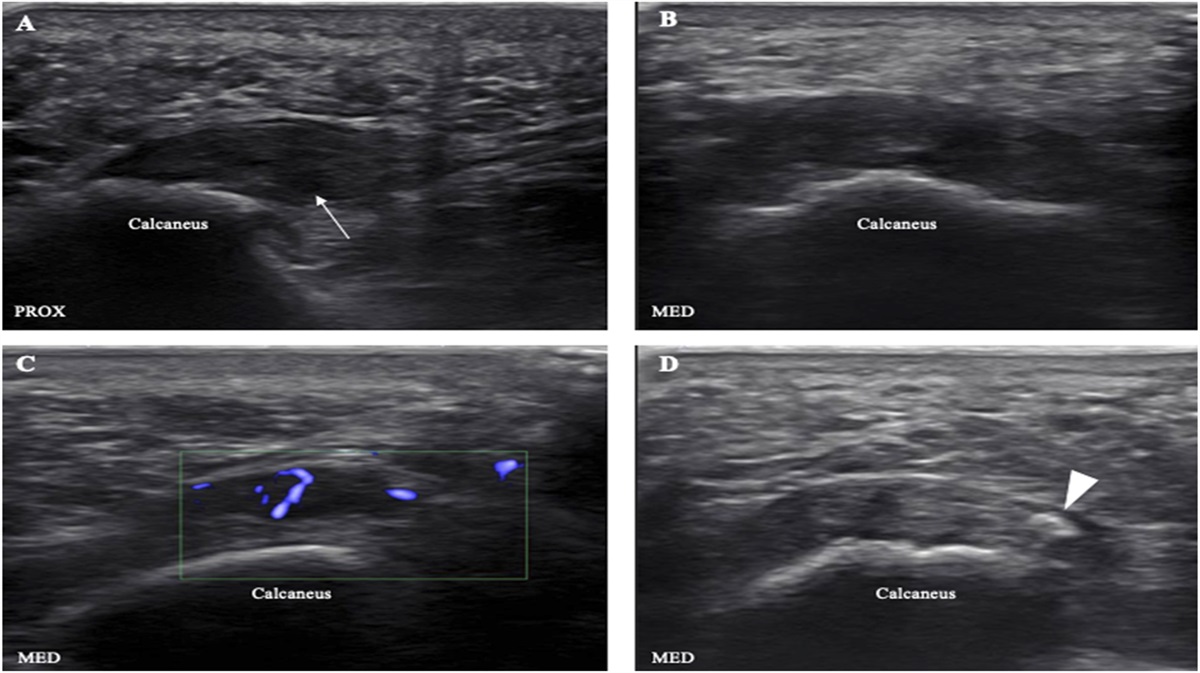
Diagnostic US examinations were performed on all patients to evaluate for plantar fascia thickening (greater than 0.4 cm9), hypoechogenicity, Doppler flow, and fiber disruption, as well as for abnormalities of the plantar fat pad (Figure 1). The ultrasonic fasciotomies were performed in a clinic-based procedure room. All patients were prepped and draped using a pristine sterile technique. Before the procedure, all patients underwent an US-guided tibial nerve block in the tarsal tunnel for regional anesthesia (Figure 2), followed by local anesthesia of the skin, subcutaneous tissues, and plantar fascia (Figure 3). Next, a #11 blade was used to make a small, horizontal stab incision at the medial heel. Then, the TX2 device was advanced to the plantar fascia under the guidance of US with an in-plane, medial-to-lateral approach. Using both short and long-axis orthogonal views of the plantar fascia, the pathologic tissue was debrided and removed (Figure 4). After the procedure, the wound was closed with Steri-Strips (3M, St. Paul, MN) and a Tegaderm occlusive bandage (3M, St. Paul, MN).
Common sonographic abnormalities of the plantar fascia. A, Long-axis view of a thickened, tendinopathic central cord origin with a partial-thickness tear of the deep fascial origin (white arrow). B, Short-axis view of a tendinopathic plantar fascia. C, Short-axis view of the plantar showing intrafascial Doppler. D, Short-axis view of the plantar fascia, with an intrafascial calcification of the lateral cord (white arrowhead). MED, medial; PROX, proximal.

Tibial nerve (TN) block in the tarsal using an in-plane, lateral-to-medial approach. ACH, Achilles tendon; FDL, flexor digitorum longus tendon; FHL, flexor hallucis longus tendon; MM, medial malleolus; PTT, posterior tibialis tendon; TN, tibial nerve. White arrowheads = needle; asterisk = local anesthetic injectate around TN.

Infiltration of the local anesthetic into the plantar fascia. MED, medial. White arrowheads = needle.

Ultrasonic fasciotomy of the plantar fascia. A, In-plane, medial-to-lateral approach of the ultrasonic fasciotomy device with a short-axis view of the plantar fascia. B, Out-of-plane appearance of the ultrasonic fasciotomy device with a long-axis view of the plantar fascia. MED, medial; PROX, proximal; white arrowhead = ultrasonic fasciotomy device
Postprocedure Protocol
Patients were allowed to bear weight as tolerated with the use of an air cam walker boot for the first 5 to 7 days post-procedure. After that, no assistive devices were used. Postprocedure activity restrictions included nothing more than activities of daily living for the first 2 weeks, incorporation of low-impact activities (eg, walking, biking) beginning 2 week post-procedure, and gradual return to high-impact activities (eg, running) beginning 6 weeks post-procedure. In addition, patients were required to begin formal physical therapy 2 weeks post-procedure, focusing on foot and ankle range of motion, balance and proprioception, and foot intrinsic muscle strengthening.
Outcome Measures
The primary outcome measures were change in visual analog scale (VAS) at 12 weeks compared with the preprocedure baseline and patients’ self-reported satisfaction with the procedure. Secondary outcome measures included VAS at 2, 6, and 52 weeks post-procedure as well as Foot and Ankle Ability Measure (FAAM) and Patient-Reported Outcome Measurement Information System Physical Function (PROMIS PF) scores at 6, 12, and 52 weeks post-procedure.
Data Analysis
Baseline demographics and baseline US findings were analyzed with descriptive statistics. Primary and secondary outcome variables were analyzed for significant change from baseline using paired t tests. A significant relationship between potential covariates and the primary outcome measure was evaluated using ordinary least squares regression.
RESULTS
68 patients were identified during the inclusion time line. One patient was excluded because of being non-English speaking, and therefore, 67 patients were ultimately included in the study. Baseline demographics are presented in Table 1. 59 male patients and 8 female patients were included in this study, with an average age of 49.4 years.
Baseline Demographics
| Age (yr) | |
| Mean (SD) | 49.4 (12.05) |
| Sex (%) | |
| Female | 59 (88.1) |
| Male | 8 (11.9) |
| BMI | |
| Mean (SD) | 34.12 (7.95) |
| Laterality (%) | |
| Left | 36 (53.7) |
| Right | 31 (46.3) |
| Duration of symptoms (mo) | 8.6 |
| Prior plantar fascia corticosteroid injection (%) | |
| Yes | 20 (29.9) |
| Prior plantar fascia ultrasonic fasciotomy (%) | |
| Yes | 2 (2.9) |
| Chronic pain syndrome (%) | |
| Yes | 2 (2.9) |
| Current smoker (%) | |
| Yes | 3 (4.5) |
| Active immunologic/rheumatologic disease (%) | |
| Yes | 4 (5.9) |
Preprocedure US findings are presented in Table 2. The average plantar fascia thickness was 0.63 cm. 45.6% of patients had sonographic abnormalities of the plantar fat pad, and 30.9% had an abnormal plantar fascia compressibility index. 70.1% of patients were found to have sonographic abnormalities involving only the central cord, 4.5% involving only the lateral cord, and 25.4% involving both the central and lateral cords.
Baseline US Findings
| Maximal plantar fascia thickness (cm) | |
| Mean (SD) | 0.63 (0.15) |
| Plantar fascia cord involvement (%) | |
| Central | 47 (70.1) |
| Lateral | 3 (4.5) |
| Both | 17 (25.4) |
| Plantar fascia hypoechogenicity (%) | |
| Yes | 67 (100) |
| Plantar fascia Doppler (%) | |
| Yes | 2 (2.9) |
| Plantar fascia tear (%) | |
| None | 45 (67.2) |
| Partial thickness | 18 (26.9) |
| Full thickness | 5 (7.5) |
| Plantar fat pad hypoechogenicity (%) | |
| Yes | 31 (46.3) |
| Plantar fat pad compressibility index (%) | |
| Abnormal | 21 (31.3) |
| Calcaneal enthesophyte (%) | |
| Yes | 38 (56.7) |
Postprocedure patient-reported outcomes are presented in Table 3. There was a statistically significant improvement in VAS compared with baseline at all follow-up time points (Figure 5). The average VAS improved from 6.57 at baseline to 0.80 at 12 weeks post-procedure (P P
Patient-Reported Outcomes After Ultrasonic Fasciotomy
| Week | VAS | FAAM | PROMIS PF |
| Average scores (SD) | |||
| 0 | 6.57 (1.60) | 53.20 (16.19) | 40.71 (5.41) |
| 2 | 4.87 (2.47) | — | — |
| 6 | 3.28 (2.42) | 69.71 (19.63) | 41.65 (5.69) |
| 12 | 0.81 (2.06) | 92.47 (16.99) | 48.38 (6.13) |
| 52 | 0.70 (2.08) | 93.93 (16.92) | 50.07 (6.27) |
| Change from baseline (P-value) | |||
| 2 | −1.70 ( | — | — |
| 6 | −3.28 ( | 16.51 ( | 0.94 (0.077) |
| 12 | −5.76 ( | 39.27 ( | 7.67 ( |
| 52 | −5.87 ( | 40.73 ( | 9.36 ( |

Individual (thin gray lines) and mean (bold blue line) VAS scores over time after ultrasonic fasciotomy.
The Foot and Ankle Ability Measure significantly improved at all follow-up visits compared with baseline (P P
No statistically significant relationship was found between any preprocedure US findings and the outcome measures.
The average procedural energy time was 2 minutes and 49 seconds. No procedural complications were noted during the duration of the study.
DISCUSSION
The most important finding in our study is that patients with plantar fasciopathy who were treated with an ultrasonic fasciotomy had significant improvement in pain and function by 12 weeks post-procedure and that those improvements were sustained up to 52 weeks post-procedure. In addition, 94% of patients reported satisfaction with their procedure at both the 12- and 52-week follow-up appointments.
There was a significant improvement in VAS and FAAM compared with baseline at all follow-ups.
A significant improvement in PROMIS PF was seen at 12 and 52 weeks post-procedure; however, there was not a significant change at week 6 post-procedure. This lack of significant improvement is not surprising. PROMIS PF measures the ability to perform certain physical activities, such as “exercise hard for half an hour” and “run or jog for 2 miles.”10,11 The patients in our study were on activity restrictions after the ultrasonic fasciotomy, which included no high-impact exercise, including running, until 6 weeks post-procedure at the earliest. As a result, they would not be expected to be able to perform many of these high-demand tasks at their 6-week follow-up, and as such we would not expect a significant change compared with baseline at that time point.
No procedural complications including bleeding, local soft-tissue infection, nerve injury, fascia rupture, or pain uncontrolled with over-the-counter analgesics were reported. This is consistent with previous studies demonstrating the excellent safety profile of an ultrasonic fasciotomy/tenotomy.8,12,13 While it is possible that procedural complications occurred and were not reported by the patients, they were specifically asked at all follow-up appointments about potential complications and also encouraged to contact the study team at any point with complications or concerns.
The procedural efficacy, patient satisfaction, and low complication rate seen in our study are consistent with other studies on ultrasonic fasciotomy for chronic plantar fasciopathy.7,8,14 In addition, similar findings have been shown for various tendinopathies in both the upper and lower limbs.13,15–18
It is important to consider the results of this study compared with surgical treatment options in the form of endoscopic or open release. The outcomes after surgical release are highly variable in the literature, with as low as only 50% of patients reporting a satisfactory outcome and an average time for complete recovery as long as 7.85 months.19–21 In addition, surgical fasciotomy has been shown to result in significantly decreased arch height, leading to decreased vertical force peaks when walking, and altered gait, which may lead to further impairment.22
The strengths of our study include the prospective study design and use of validated patient-reported outcomes. In addition, this is currently the largest prospective study on the safety and efficacy of ultrasonic fasciotomy for chronic plantar fasciopathy. There are, however, limitations to our study that should be mentioned. Our study included only patients with plantar fasciopathy. These findings may not be generalizable to other abnormalities of the plantar fascia (eg, plantar fibromatosis). Another limitation is that a single physician at a single institution performed all of the diagnostic US examinations and ultrasonic fasciotomies. Finally, our study did not find any relationship between diagnostic US examinations and outcomes. It is possible that a larger sample size may be able to detect a relationship.
CONCLUSION
Our study demonstrated that an ultrasonic fasciotomy is an effective and safe treatment option for patients with chronic plantar fasciopathy, with continued improvement and a high patient satisfaction rate 1 year post-procedure. Therefore, we conclude that ultrasonic fasciotomy should be considered before surgical intervention for patients with symptomatic plantar fasciopathy refractory to conservative treatments. While this study demonstrated promising results for patients with plantar fasciopathy, the use of ultrasonic fasciotomy for other disorders of the plantar fascia needs to be formally investigated.
ACKNOWLEDGMENTS
Krit Petrachaianan, BA, and Natalie Glass, PhD, for their excellent statistical support on this manuscript.
References