INTRODUCTION
Rhabdomyolysis is a condition where muscle cells break down and release myoglobin and other cellular contents. It can be caused by various factors, such as traumatic crush injuries, dehydration, medication, toxins, sepsis, hyperthermia, electrocution, overtraining, and excessive exercise. The increasing popularity of electrical muscle stimulation (EMS) training has also led to growing reports of rhabdomyolysis.1 Although individuals with underlying myopathy are at higher risk, rhabdomyolysis can also occur in highly trained athletes who engage in intense exercise or unaccustomed EMS training. The release of cellular contents potentially leads to kidney damage and compartment syndrome.
This case report describes a 46-year-old Caucasian female professional athlete with a history of kidney disease and chronic pain conditions, including fibromyalgia, chronic fatigue syndrome, and myofascial disorder, who developed rhabdomyolysis and compartment syndrome following a single session of EMS training.
CASE REPORT
The patient decided to try EMS for the first time in the hopes of alleviating her chronic pain conditions. She has a history of kidney disease secondary to hydronephrosis caused by urolithiasis, which was diagnosed in 2020. It was managed conservatively with traditional Chinese medicine and increased water intake. She also has multiple chronic pain conditions diagnosed in 2003, which she has been managing with various medications and physical exercise. On April 19, 2022, the patient underwent a full-body EMS treatment with high-intensity settings (electrodes were fitted bilaterally over the arms, stomach, chest, upper and lower back, thighs, and glutes) with Magicox company (Xi’an, PR China). During the course of exercise, the patient experienced moderate discomfort, prompting her to inform the personal trainer. Despite her reaction, the personal trainer instructed her to perform basic full-body exercises for an hour, while keeping the EMS unit at the maximum level (large pulses between 300 and 450 μs, high frequency 50–100 Hz), which was deemed suitable for a professional athlete. Following the session, she experienced fatigue and immediate-onset muscle soreness in various areas of her body. Over the next few days, the muscle soreness spread and caused significant swelling in the buttocks, along with mild decreased sensation and paresthesia in the sciatic nerve distribution areas, which prompted her to visit our hospital.
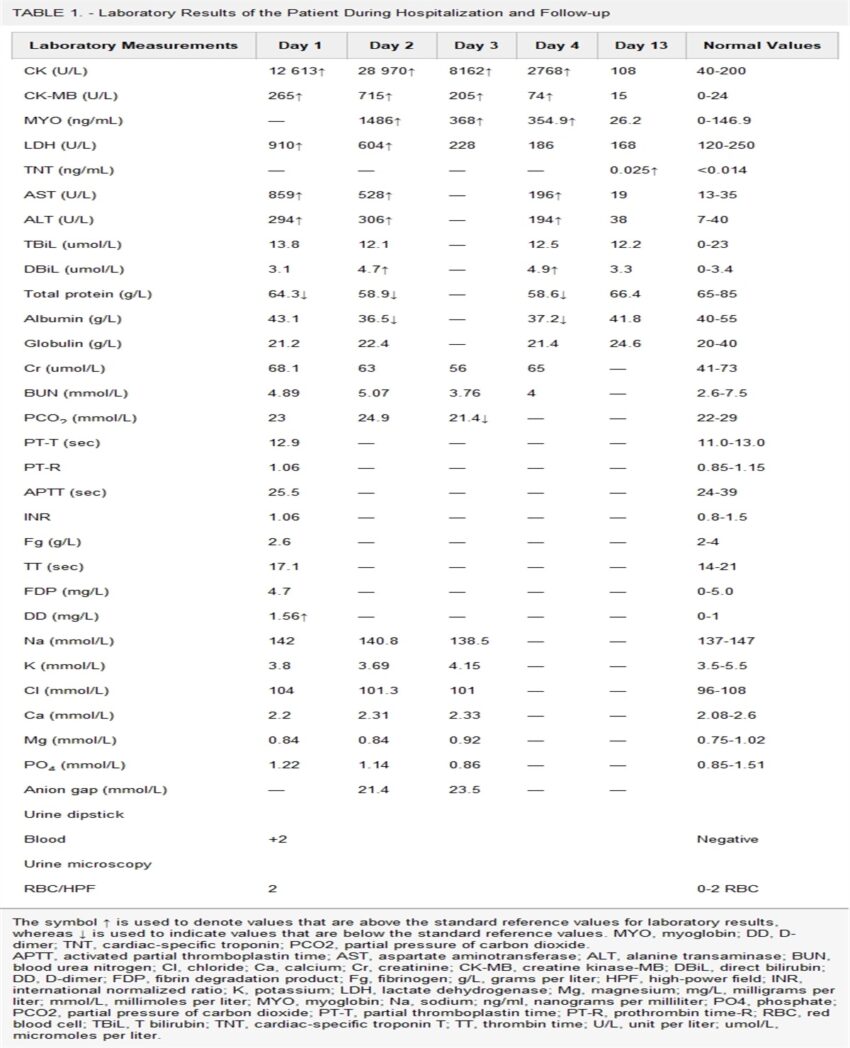
On presentation, the patient’s vital signs were stable with a blood pressure of 129/62 mm Hg, a resting heart rate of 107 beats per minute, a respiratory rate of 20 breaths per minute, and a body temperature of 36 °C. Her oxygen saturation was 97% under atmospheric air. She had moderate swelling and tenderness in the thighs and gluteal region, but no weakness was observed in her lower extremities. Her pain level upon admission on a numeric pain rating scale was an 8.5 out of 10. Laboratory tests revealed elevated creatine kinase (CK), CK-MB, and lactate dehydrogenase (LDH) levels, indicating rhabdomyolysis (Table 1). The patient was hospitalized and received intensive intravenous fluid therapy and sodium bicarbonate supplementation to flush out myoglobin and prevent kidney damage.
Laboratory Results of the Patient During Hospitalization and Follow-up
| Laboratory Measurements | Day 1 | Day 2 | Day 3 | Day 4 | Day 13 | Normal Values |
| CK (U/L) | 12 613↑ | 28 970↑ | 8162↑ | 2768↑ | 108 | 40-200 |
| CK-MB (U/L) | 265↑ | 715↑ | 205↑ | 74↑ | 15 | 0-24 |
| MYO (ng/mL) | — | 1486↑ | 368↑ | 354.9↑ | 26.2 | 0-146.9 |
| LDH (U/L) | 910↑ | 604↑ | 228 | 186 | 168 | 120-250 |
| TNT (ng/mL) | — | — | — | — | 0.025↑ | |
| AST (U/L) | 859↑ | 528↑ | — | 196↑ | 19 | 13-35 |
| ALT (U/L) | 294↑ | 306↑ | — | 194↑ | 38 | 7-40 |
| TBiL (umol/L) | 13.8 | 12.1 | — | 12.5 | 12.2 | 0-23 |
| DBiL (umol/L) | 3.1 | 4.7↑ | — | 4.9↑ | 3.3 | 0-3.4 |
| Total protein (g/L) | 64.3↓ | 58.9↓ | — | 58.6↓ | 66.4 | 65-85 |
| Albumin (g/L) | 43.1 | 36.5↓ | — | 37.2↓ | 41.8 | 40-55 |
| Globulin (g/L) | 21.2 | 22.4 | — | 21.4 | 24.6 | 20-40 |
| Cr (umol/L) | 68.1 | 63 | 56 | 65 | — | 41-73 |
| BUN (mmol/L) | 4.89 | 5.07 | 3.76 | 4 | — | 2.6-7.5 |
| PCO2 (mmol/L) | 23 | 24.9 | 21.4↓ | — | — | 22-29 |
| PT-T (sec) | 12.9 | — | — | — | — | 11.0-13.0 |
| PT-R | 1.06 | — | — | — | — | 0.85-1.15 |
| APTT (sec) | 25.5 | — | — | — | — | 24-39 |
| INR | 1.06 | — | — | — | — | 0.8-1.5 |
| Fg (g/L) | 2.6 | — | — | — | — | 2-4 |
| TT (sec) | 17.1 | — | — | — | — | 14-21 |
| FDP (mg/L) | 4.7 | — | — | — | — | 0-5.0 |
| DD (mg/L) | 1.56↑ | — | — | — | — | 0-1 |
| Na (mmol/L) | 142 | 140.8 | 138.5 | — | — | 137-147 |
| K (mmol/L) | 3.8 | 3.69 | 4.15 | — | — | 3.5-5.5 |
| Cl (mmol/L) | 104 | 101.3 | 101 | — | — | 96-108 |
| Ca (mmol/L) | 2.2 | 2.31 | 2.33 | — | — | 2.08-2.6 |
| Mg (mmol/L) | 0.84 | 0.84 | 0.92 | — | — | 0.75-1.02 |
| PO4 (mmol/L) | 1.22 | 1.14 | 0.86 | — | — | 0.85-1.51 |
| Anion gap (mmol/L) | — | 21.4 | 23.5 | — | — | |
| Urine dipstick | ||||||
| Blood | +2 | Negative | ||||
| Urine microscopy | ||||||
| RBC/HPF | 2 | 0-2 RBC |
The symbol ↑ is used to denote values that are above the standard reference values for laboratory results, whereas ↓ is used to indicate values that are below the standard reference values. MYO, myoglobin; DD, D-dimer; TNT, cardiac-specific troponin; PCO2, partial pressure of carbon dioxide.
APTT, activated partial thromboplastin time; AST, aspartate aminotransferase; ALT, alanine transaminase; BUN, blood urea nitrogen; Cl, chloride; Ca, calcium; Cr, creatinine; CK-MB, creatine kinase-MB; DBiL, direct bilirubin; DD, D-dimer; FDP, fibrin degradation product; Fg, fibrinogen; g/L, grams per liter; HPF, high-power field; INR, international normalized ratio; K, potassium; LDH, lactate dehydrogenase; Mg, magnesium; mg/L, milligrams per liter; mmol/L, millimoles per liter; MYO, myoglobin; Na, sodium; ng/ml, nanograms per milliliter; PO4, phosphate; PCO2, partial pressure of carbon dioxide; PT-T, partial thromboplastin time; PT-R, prothrombin time-R; RBC, red blood cell; TBiL, T bilirubin; TNT, cardiac-specific troponin T; TT, thrombin time; U/L, unit per liter; umol/L, micromoles per liter.
During her hospital stay, the patient’s CK and myoglobin levels gradually decreased (Table 1), and her symptoms improved. She was discharged on the fifth day of admission against medical advice, although she had mildly elevated troponin on a follow-up investigation a week later. The mild increase in troponin level was possibly due to a noncardiovascular cause, as she had no symptoms of myocardial injury. The troponin level normalized over a 2-week period.
DISCUSSION
Electrical muscle stimulation therapy is a technique that uses wearable devices to increase muscle contractions by using low- and mid-frequency electric currents. Electrical muscle stimulation works by sending electrical impulses to the nerves that innervate muscles, generating action potential that mimics the signal typically coming from the central nervous system, causing the muscles to contract and relax.2 EMS training can have various benefits, such as increasing muscle strength, improving body composition, and reducing lower back pain in people with chronic back pain.3–5 However, individuals with underlying myopathy and certain medical conditions, such as thyroid disorders, uncontrolled diabetes, and chronic kidney disease, are predisposed for developing rhabdomyolysis and its complications.6–8 Therefore, it is important to exercise caution and carefully assess the medical history of individuals before starting EMS training.
The primary approach for managing rhabdomyolysis involves correcting intravascular volume depletion and preventing the formation of intratubular casts with aggressive fluid resuscitation. Normal saline and lactated Ringer solution are commonly used to maintain adequate hydration and flush out myoglobin while ensuring a sufficient urine output. Electrolyte imbalances should also be closely monitored and addressed, and urinary alkalization with sodium bicarbonate can help minimize kidney damage caused by myoglobin. Loop diuretics may be beneficial in patients with fluid overload while increasing tubular flow and reducing the risk of myoglobin precipitation.9
Disruption of skeletal muscle integrity, inflammation, and fluid accumulation associated with rhabdomyolysis can lead to increased pressure within compartments and the development of compartment syndrome. In cases of acute compartment syndrome, surgical decompression may be necessary to prevent nerve damage when there is a significant increase in compartment pressure and signs of ongoing tissue damage or neurovascular compromise. Gluteal compartment syndrome is a rare condition that can cause disability if treatment is delayed, characterized by buttock swelling, pain, and potential nerve damage. Direct measurement of compartment pressure is crucial for diagnosis. Although fasciotomy reduces pressure, it does not significantly affect long-term neurological deficits or mortality in gluteal compartment syndrome and carries risks of bleeding, infection, and scarring.10 For mild gluteal compartment syndrome, conservative management can be successful if symptoms are not severe enough to warrant surgery. The patient in our case had gradual improvement without neurological deficits or sequelae.
It is important to note that adaptation to exercise and gradual exposure to EMS training can help reduce the risk of muscle damage and rhabdomyolysis.11 Exercise adaptation reduces muscle damage and is demonstrated by lower blood CK levels. Some studies have also demonstrated high-frequency EMS training leads to more muscle damage compared with low-frequency training.12,13 Individuals with no previous experience in EMS training should start with low-intensity and low-frequency exercises to allow their muscles to adapt before progressing to higher intensities and frequencies. Furthermore, individuals with chronic diseases and myopathies should avoid EMS training to prevent potential complications. In this patient, the presence of underlying myopathy together with her involvement in EMS training under a high-frequency setting predisposed her to rhabdomyolysis. Therefore, it is crucial to note that EMS is a medical modality that requires proper training and supervision. It should only be performed by medical professionals who are adequately trained on the use, risks, and benefits of this modality.
In conclusion, EMS training carries an increased risk of severe complications, including rhabdomyolysis, particularly in individuals with underlying risk factors. A cautious approach is necessary when considering EMS training for beginners, and their medical history should be thoroughly evaluated. Moreover, further research, particularly high-quality randomized controlled trials, is needed to establish safe and validated EMS training protocols tailored to individual needs and the risk of complications.
References